Pericardial Effusion & Tamponade
Pericardial fluid and the diagnosis of tamponade demonstrated through two patient cases.
Pericardial effusion (PCE) is important both in the hospital and clinic. We must be competent at detecting pericardial tamponade (PT) because this determines how rapidly we must act.
DETECTING PCE
PCE can be free-flowing or loculated; all cardiac views are needed to detect and size the PCE. The anechoic fluid of PCE must be differentiated from epicardial fat, which follows the normal motion of the pericardium, has some echogenicity, is typically <1cm in thickness, and is most frequently seen around the right heart. The subcostal4 view, particularly with a more upright patient, should be the most sensitive way to image free-flowing pericardial effusion. The rest of this chapter focuses on tamponade.
TAMPONADE
PT can present insidiously and nonspecifically in the clinic. Patients with severe PT (hypotension, ≥ 2 cm wide effusion, a swinging heart, and collapsing RA and RV) usually are sick and go right to the hospital. They are not a diagnostic challenge if the views are good. Identifying subtler PT in less ill patients requires more knowledge and skill. PT was diagnosed in two clinic patients within several weeks of each other, and together, they demonstrated the diagnostic issues. These two cases are presented after summarizing important points about tamponade.
SUMMARY POINTS
A. Fluid in the pericardium increases the pressure on the heart. Acute fluid raises the pressure quickly, while slowly accumulating fluid produces a more gradual rise in pressure. Thus, the amount of fluid cannot reliably predict intrapericardial pressure. A swinging heart in a large effusion is almost always associated with hemodynamic compromise.
B. When intrapericardial pressure becomes higher than the diastolic pressure in any chamber, the chamber collapses during diastole. Diastolic pressure is lowest in the RA, followed by the RV, LA, and LV. Most clinic patients would be seen when only RA or RA + RV diastolic collapse is occurring.
C. Look carefully for RA and RV diastolic collapse with a view (preferably the subcostal4) showing both the RV and RA and freeze it. Play the clip in slow motion and observe for inward RA wall movement at the beginning of RV systole, when RA pressure is lowest. RV diastolic collapse occurs as the TV is opening. The following patient had a large effusion and obvious RA collapse.
The following shows both RA and RV diastolic collapse.
D. The IVS can shift toward the LV with inspiration (increased interventricular dependence) with more substantial PT. It may take various views to see this change with inspiration. Notice the intermittent bounce of the IVS toward the LV in the clip just above. The physician noted that this occurred with inspiration.
E. An increased difference in the E velocity between expiration and inspiration is a traditional marker for PT. However, false positives can occur if respiratory, heart, or examiner finger movement causes the Doppler gate to move in and out of the optimal position. If an LV inflow tracing is steady throughout inspiration and expiration with E variation under 20%, the chance of meaningful PT is very low.
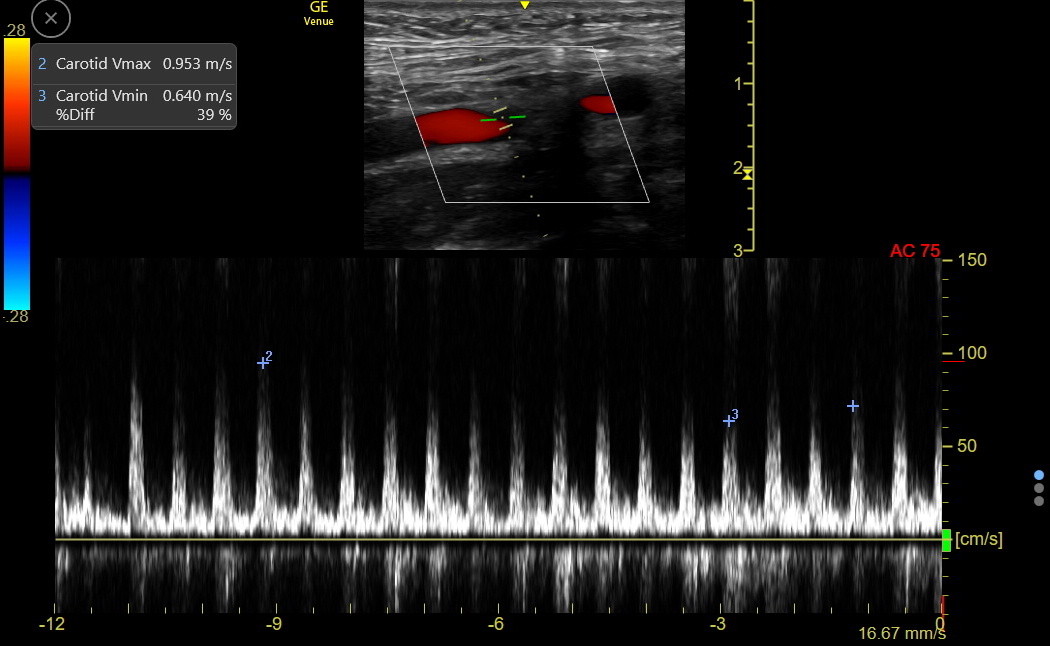
F. Variation in the carotid peak PW velocity with respiration is a marker of PT that reduces confounding from motion. A peak velocity difference between inspiration and expiration greater than 20-25% is suspicious for PT. However, there are still unusual false positives and negatives with this measurement:
False positives: COPD, mucus plug, pneumothorax, PE, upper airway obstruction
False negatives: positive pressure ventilation, severe AR, large ASD, severe LV hypertrophy, severe LV dysfunction with elevated end-diastolic pressure, and intravascular volume depletion.
The carotid velocity tracing from the patient above shows 39% respiratory variation.
G. Increased JVP with a Kussmaul sign will be seen when the RA pressure is high enough. A Kussmaul IJ is shown in the first PT patient described below.
H. Significant PT usually distends the IVC, rounds its shape, and reduces the inspiratory collapse. The following IVC clip is from the patient just above. The IVC is about 2 cm and has minimal respiratory collapse.
A PCE that is modest in size with normal inspiratory septal motion, no hint of RA collapse, and normal respiratory variation in E or carotid velocity can be seen back in clinic in a handful of days to be sure the PCE is not expanding. If such a patient seems systemically ill, the interval to repeat the examination should be shorter.
A moderate or greater size PCE with any of the markers of hemodynamic compromise needs referral to the ED to facilitate early echocardiography and cardiology consultation.
PATIENT 1:
A mitral valve was repaired, and the patient did well for several weeks but then noticed an increased heart rate, decreased appetite, and a little more shortness of breath during cardiac rehab. Here is how the IMBUS exam happened in the clinic.
Given the symptoms, the physician looked first at the JVP. He noticed that the patient’s JVP was periodically elevated but only during inspiration, which is a positive Kussmaul sign indicating a compromised right side of the heart. The beginning of the following clip shows the IJ vein distended at peak inspiration and then collapsed as the patient exhaled.
The patient then had cardiac IMBUS, starting with the PLAX view. As shown in the following clip, the patient was tachycardic, and systolic function appeared at least mildly/moderately reduced, which would be typical after a mitral valve repair. The mitral valve looked intact, and color flow Doppler showed no mitral regurgitation. The distinctive hyperechoic structure bulging into the LA with a subtle double bounce was not immediately explainable. Notably, pericardial effusion was not of a significant volume in the PLAX.
The PSAX was next, and while it was only a fair view, it was suspicious for a pericardial effusion at the lower left. In addition, about ¾ of the way through the clip, the LV becomes more apparent, with an unusual bounce to the septum that seemed to happen with inspiration. This increased interventricular dependence alerted the physician to possible PT, but the lack of clear-cut PCE was puzzling.
The apical4 was next, of fair quality, and, significantly, slightly rotated out of plane. It was suspicious for a PCE outside the RA and RV. A few glimpses suggested that the RV might have collapsed (exaggerated by the slightly rotated out-of-plane image making the RV look smaller), and the septum again seemed to shift to the left intermittently.
The physician then slid the probe a little lateral around the apex to a partial RV-enhanced view, and then the PCE was more apparent. The RV continued to look like it was collapsing, but the views continued suboptimal and slightly off rotation.
Being very concerned about PT, the physician rotated the probe towards an apical3 view and angled slightly toward the right side. The bulging structure into the LA was seen as a portion of pericardial fluid connected to the more considerable effusion and bowing in the left atrial wall at the end-diastole. This indicated that the pressure in the pericardial sack was becoming greater than the lowest LAP. This was a dangerous sign. The PCE and the RV were hard to distinguish.
Hoping for further clarification, the physician went to the subcostal view. Now, the PCE was obvious and about 3 cm wide on top (the inferior heart) and about 1.5-2 cm at the bottom (the superior heart). The RV again seemed to be collapsing.
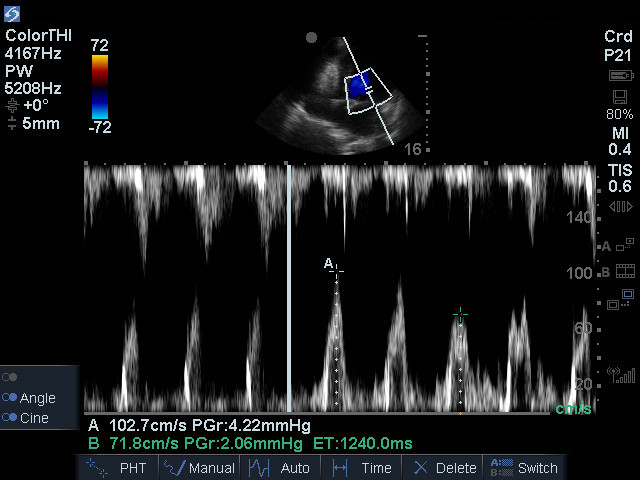
As a final measure to investigate PT, the physician returned to the apical4 view and performed mitral inflow analysis with pulse wave Doppler. He changed the sweep speed to SLOW so many complexes would accumulate on the screen. He watched while the patient was inspired and then expired. He froze the screen to show the higher peak mitral inflow velocity with expiration, followed by the lower peak velocity with inspiration. The patient was in sinus rhythm, so the single complex is a fused E/A wave because of tachycardia. Because the patient’s heart was not swinging very much (swinging results in the interrogation location/angle, and thus measured peak velocity, changing from beat to beat), the variation of the E wave with inspiration is a measure of PT. In this patient, there was a 30% decrease in peak E velocity with inspiration. Over 25% is abnormal, and 30% is highly likely to be PT. The potential false positive error with this method comes when the normal respiratory movement of the heart moves the Doppler gate in and out of the optimal flow position.
This first patient was urgently admitted and confirmed to have PT; 140 mL of bloody fluid was withdrawn, and the patient felt better. However, the fluid reaccumulated the next day, and it was decided that the patient needed a surgical drainage procedure to prevent pericardial constriction. The pericardial effusion was not infectious but just an inflammatory complication of the cardiac surgery.
PATIENT 2:
This patient had received a right pneumonectomy years ago for lung cancer. He had done well and was in for an annual physical. Reviewing symptoms, he mentioned that his breathing had worsened over the last few weeks. This prompted cardiopulmonary IMBUS.
The JVP might have helped but wasn’t evaluated because the physician thought there was going to be a pulmonary problem because the patient had no previous cardiac disease. The right side of the chest had no lung, and nothing was seen with IMBUS. However, a mild to moderate pleural effusion was on the left side. Cardiac IMBUS was then performed.
This was an unusual and challenging exam because the complete right pneumonectomy had shifted the heart to the right. There was nothing in the standard left parasternal or apical windows. The physician then moved the patient supine and looked for a view in the right parasternal area. The view was not good, but the clip shows that with a PSAX-type view, there was clearly a PCE, and the septum was intermittently pushed into the LV, which was seen to happen with inspiration.
The suspicion of PCE with PT was now high, so the physician hunted lower along the left sternal border for something that might be an apical4 and got this poor view. It appeared to show a reasonably large PCE with a swinging heart.
Finally, the physician worked subcostal, angling towards the right chest. It was then definite that there was at least a moderate-sized PCE with the RA and RV collapsing.
The physician knew there was an emergency, and this patient was urgently admitted and quickly drained of 300 mL of bloody fluid. He felt much better, and his hemodynamics improved. At the time of the procedure, the pressure in the pericardium measured 15 mmHg, indicating PT. Despite the concern about recurrent lung cancer, cytology was negative on the fluid, and the etiology of the fluid remained unclear.