Right Ventricular Size & Function
An overview of right ventricular size and functional assessment
This chapter covers the basics of RV size and function, but the Advanced Right Heart chapter covers additional views and how they are used with some essential but more unusual right heart diseases.
Right ventricular filling and output are maximal toward the end of inspiration when most measurements should be taken. However, this may be when some views are the poorest, so use the best view and accept the compromise. Some aspects of RV size and function vary with body height.
RIGHT VENTRICULAR SIZE
It is harder to evaluate RV size than LV size. The RV sits primarily behind the sternum, so the views can be challenging. The RV shape is also complicated, with the inflow and outflow portions at an angle to each other, resembling a bagpipe. The RV is first seen in the PLAX when the proximal part of the RV outflow tract (RVOT) is imaged. The typical shape of the posterior border of the RVOT in this view is a bit triangular; seeing a rounded lower border is a hint of RV troubles. Measuring the diameter of the RVOT in this view is possible but can be falsely enlarged because the cut through the RVOT is oblique. Here is a PLAX with a reasonably normal RVOT shape.
Next is a PLAX from a patient with RV dilation. The shape is subtly rounder, but the RVOT does not appear larger relative to the aorta or the left atria because both were also dilated in the patient. Thus, the 1/3, 1/3, 1/3 rule for eyeballing the RVOT, aorta, and left atrium size can fail. The PLAXR gives a better visual estimate of RV size.
The RV size is eyeballed in the apical4 if we know that the LV size is normal. The part of the RV seen in the apical4 should usually appear around 1/3 smaller than the LV. Use an RV-enhanced view if the RV lateral wall is uncertain. Two tricuspid valve leaflets need to be seen for a correct RV view. A normal RV is triangular-shaped (shark fin) in the apical4, with a larger basal than mid-RV diameter. Measuring the basal diameter is good enough in most IMBUS clinical situations because the RV enlargement is diffuse. Here is an apical4 of a dilated RV with severe tricuspid regurgitation. The RV was visually larger than the LV, and the mid-RV diameter measured 4.5 cm, which is severely enlarged (see the table below).
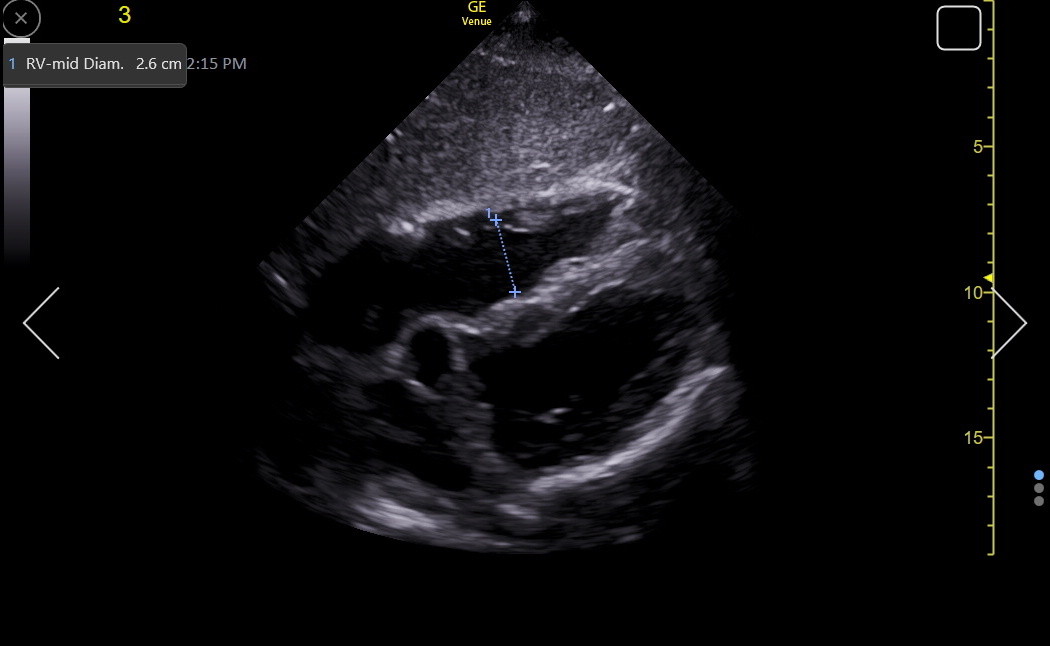
A good subcostal view can confirm RV dilation because the beam is more perpendicular to the RV walls. Here is a normal mid-RVEDD in SC4.
When we know that the IVS is normal in a patient, we can eyeball the basal RV lateral wall and note whether it is less than half the diameter of the IVS. Even with an optimized SC4, precisely measuring a normal lateral wall is challenging. Decreasing the depth (and perhaps width) and moving the focus position to the RV lateral wall can help improve wall definition. Because the RV is closer to the transducer in this view, increasing the frequency to RES is a final adjustment that can improve wall resolution. Don’t include the pericardium or any epicardial fat pad in a measurement. The following is an image from a patient with pulmonary hypertension who had hypertrophy of the lateral wall. A more precise measurement would have been obtained with a more optimized view, but by eyeball, the lateral wall was as thick as the IVS.
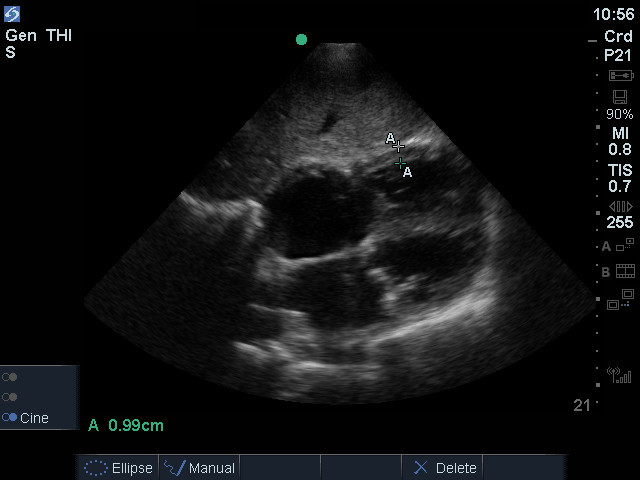
Measuring the RV lateral wall in patients with substantial hepatic steatosis may be difficult. The right ventricle is also strongly trabeculated; including trabeculae or chordae in the measurement will falsely increase it. Measuring in the first part of the basal RV usually avoids this confusion.
RV dimensions (cm) |
Normal |
Mild |
Mod |
Severe |
Mid RV |
1.9 - 3.5 |
3.5 - 3.7 |
3.8 - 4.1 |
≥ 4.2 |
RV lateral wall |
0.1 - 0.6 |
|
|
|
RIGHT VENTRICULAR FUNCTION
An indicator of RV volume and pressure overload is flattening (D-ing) of the interventricular septum toward the LV, as relatively increased RV pressure distorts the LV. This can be seen in any view that shows both ventricles and the IVS. When RV volume overload is the problem, flattening occurs more during diastole, while RV pressure overload causes more flattening during systole. With pericardial tamponade, the fattening may initially occur just during inspiration. The next PSAX shows prominent septal flattening.
RV function has a more significant component of longitudinal contraction than LV function. However, it is still essential to eyeball the radial function as the RV is imaged. The longitudinal function of the basal RV is traditionally measured with M-mode tricuspid annular plane systolic excursion (TAPSE), which is obtained at the lateral TV annulus like the mitral annulus MAPSE that was discussed in the LV Size and Function chapter. However, TDI s’ of the TV annulus is a better measure of longitudinal function because TAPSE tends to overestimate longitudinal function. With Venue, it is also quicker to obtain s’ than TAPSE. In the following patient, anatomic M-mode was used to measure a normal TAPSE. Normal movement of the TV annulus is usually easy to eyeball after enough training.
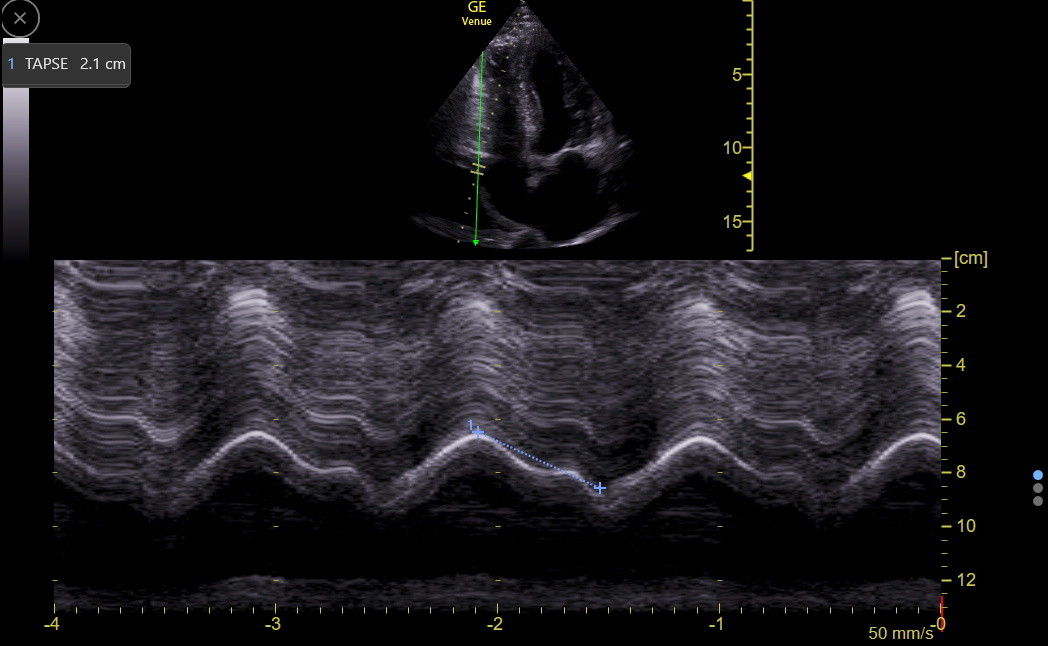
|
Normal |
TAPSE (cm) |
1.7 - 3.1 |
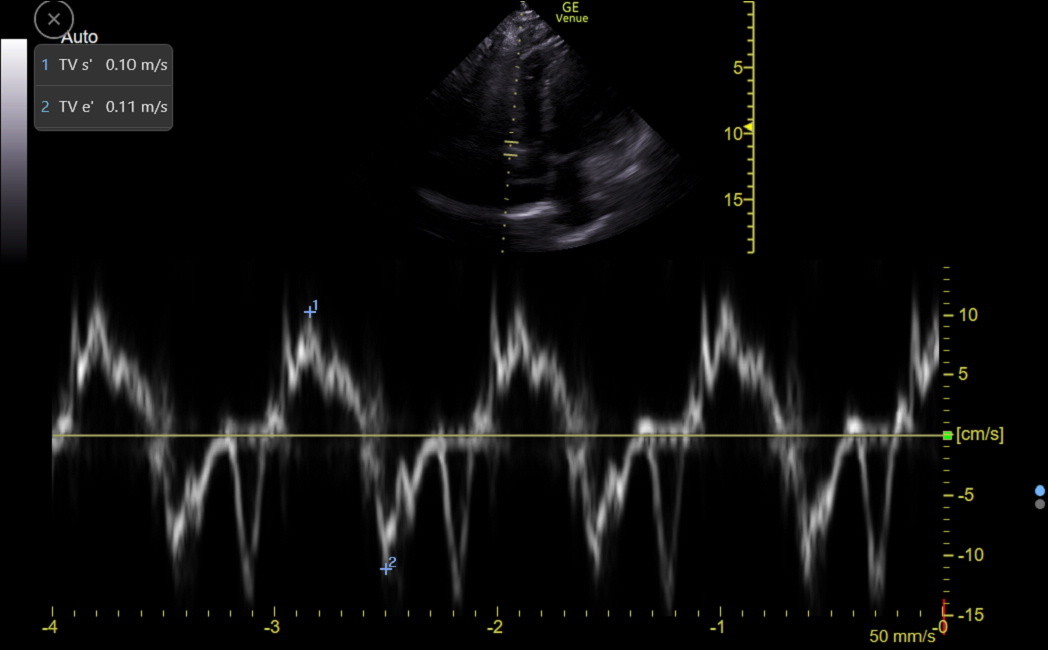
An s’ of the TV lateral annulus ≥ 0.10 m/sec is a strong marker of preserved basal RV longitudinal function in middle-aged and elderly patients and indicates the absence of severe pulmonary hypertension (Saxena, Echocardiography 2006;23:750-5). Here is a normal TDI tracing of the lateral TV annulus with both s’ and e’ measured.
TV e’ reflects RV diastolic function, but isolated RV diastolic dysfunction is rare, so TV e’ isn’t usually measured. However, TV e’ can help assess right atrial pressure, as discussed in the following Atrial Size and Function chapter.
While TAPSE and TV s’ are measures of longitudinal RV function, they are specific to the base of the RV. If RV dysfunction is localized to more distal parts of the RV, TAPSE and TV s’ will be falsely reassuring(see the Advanced Right Heart Disease chapter).