Bladder and Pelvis
The utility of being able to gain information from a subset of pelvic structures is important in both the inpatient and outpatient setting.
BLADDER
The urinary bladder lies extraperitoneal and immediately cephalad to the pubic bone. It is a critical structure and an acoustic window to see reproductive organs and the posterior pelvic space. Details of these extra-bladder structures are discussed later in this chapter.
It is better to systematically examine all aspects of the bladder in the transverse and longitudinal planes and then go back and examine the structures posterior to the bladder as a separate task. The following anatomy is pertinent.
IMAGING THE BLADDER
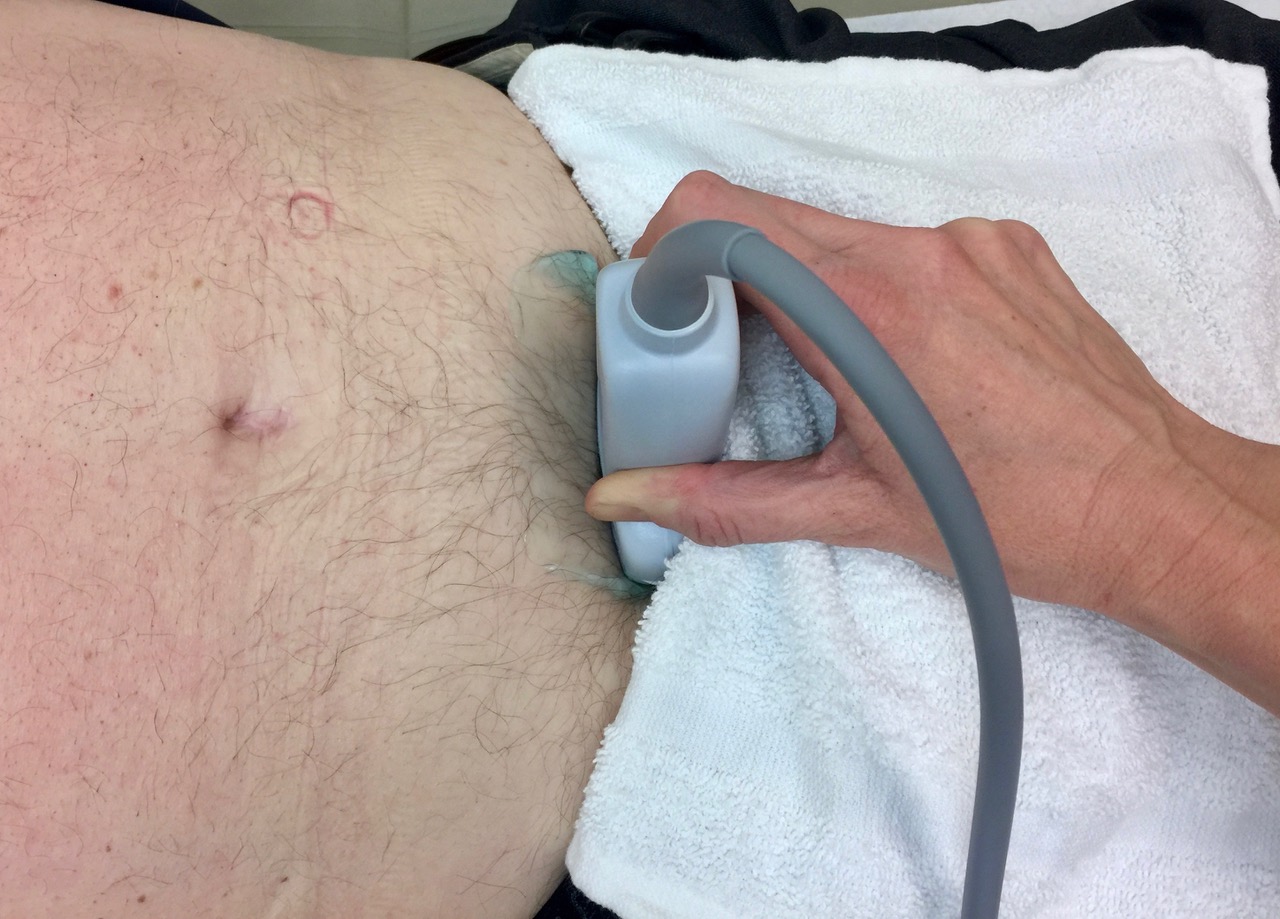
Use the curvilinear probe. The supine position is best for most exams, but a semi-upright position is more sensitive to pelvic abdominal fluid. Be careful with pressure on the bladder at the start because a full bladder may be uncomfortable. Drape the patient’s undergarments with a washcloth.
Optimization: Details of the bladder wall must be seen, so adjust the depth and move the focus position to the middle of the bladder. Make sure the gain shows urine as anechoic. There may be some hyperechoic artifacts near the anterior wall of a bladder, but these can be reduced with the TGC control.
Transverse View: Place the probe immediately cephalad to the pubis with the indicator physician left.
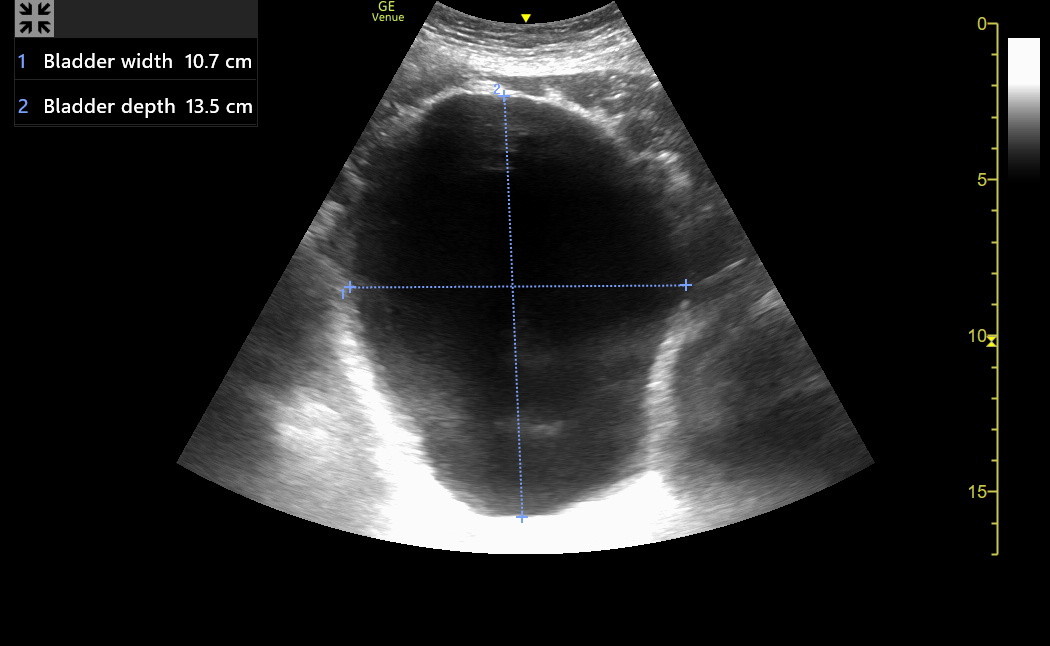
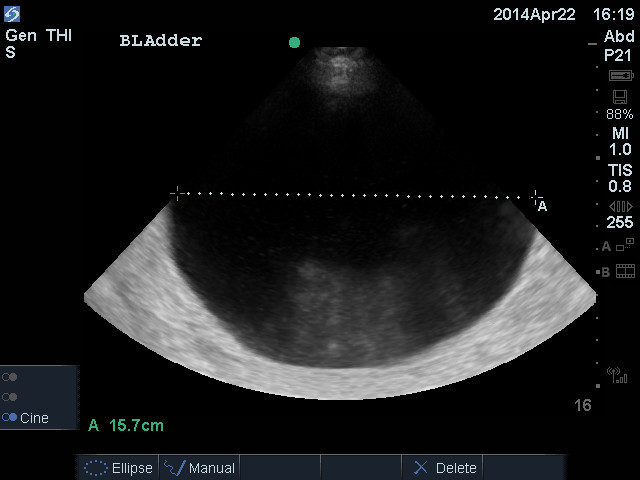
Most bladders will be immediately seen, but caudad fanning may be needed for very small bladders. Here is a distended bladder in transverse view. Notice the modest artifact below the anterior wall and the intense posterior acoustic enhancement because of the large urine volume.
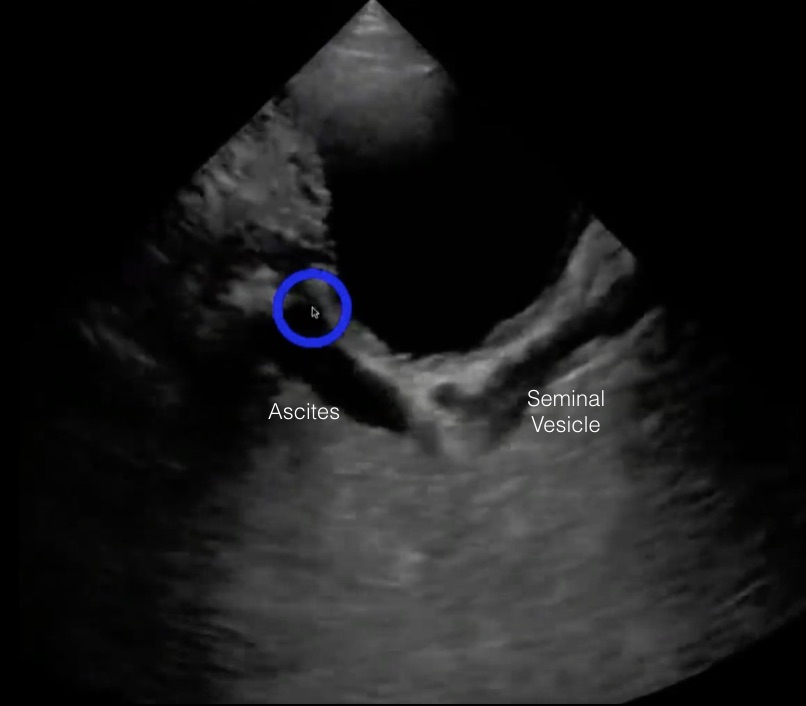
Trap: Next is a patient with prominent ascites and a Foley catheter. An initial suspicion was a full bladder with a plugged Foley.
The distinctive fluid-filled Foley catheter bulb is visible posterior to the anechoic fluid. A variety of abdominal views in this patient showed a large amount of ascites. The ascites had pushed the collapsed bladder against the symphysis pubis and down into the pelvis on top of the Foley. Notice the thin layer of fluid under the Foley. This is ascites in the rectovesicular space (this could be a man or a woman with a hysterectomy), as shown in the following diagram.
The rectovesicular and rectouterine spaces are sensitive to intraperitoneal fluid, particularly with a partially upright patient. The sagittal view is best to see this fluid. The transverse view in males may misinterpret the seminal vesicles (lateral and retroperitoneal) as ascites. The parasagittal view avoids these structures.
Transverse bladder dimensions: Find the image where the transverse bladder appears the largest and Freeze. Measure the lumen WIDTH (left to right on the screen, halfway down the bladder) and the DEPTH (top to bottom), as was done in the transverse distended bladder image above.
Bladder distortion: A large uterus or prostate may push the posterior wall of the bladder anteriorly; measure through this bulge to the depth of the posterior wall seen on each side of the bulge.
After measuring the transverse bladder and storing the image, carefully slide/fan cephalad to caudad through the bladder, looking for wall abnormalities.
Bladder jets: Bladder jets may be seen easily in the transverse view or only with searching and waiting (several minutes is a practical maximum). The ureters drain into the bladder near the beginning of the urethra in the bladder trigone. This is located on the posterior and more caudad wall of the bladder. However, as the bladder distends, the ureters spread apart and away from the urethra. They remain posterior but may move more cephalad. The best probe position is over the cephalad bladder, with the beam angled diagonally to the posterior caudad wall. This plane should pass through jets entering the bladder. Here is a patient with only a modestly full bladder and a jet easily seen in B-mode with a lucky parasagittal position.
Power Doppler Imaging (PDI) can enhance the jets, as seen in the following woman with mild right hydronephrosis from a stone. Only a left-sided bladder jet was seen. PDI is more sensitive to flow than Color Doppler.
Bladder jets are helpful in patients with possible unilateral hydronephrosis. A visualized bladder jet on a suspect side indicates that the ureter is not entirely blocked, making the situation non-urgent. An absent jet implies a likely obstructed ureter and the need for more urgent intervention.
A kidney stone stuck at the ureteral-vesicular junction can be visualized in the posterior wall. In addition, Color and PDI have shown a characteristic twinkling artifact over the stone. The following was taken from a 5 Min Sono podcast discussing a patient with right-sided hydronephrosis. Color was applied, and twinkling was seen where a stone was stuck, indicating an uneven, calcified surface.
Longitudinal bladder shape and length: Rotate the probe to the sagittal position, make the bladder as large as possible, and tilt the probe to bring in the caudad wall. The shape of the bladder in the longitudinal orientation is variable. Normal, moderately full bladders often appear somewhat triangular, while very full bladders may appear ellipsoid or cuboid. A standard measurement technique is needed for the cephalad-caudad LENGTH of the bladder, and the best is probably to measure the horizontal cephalad-caudad dimension through the middle of the bladder, regardless of its shape.
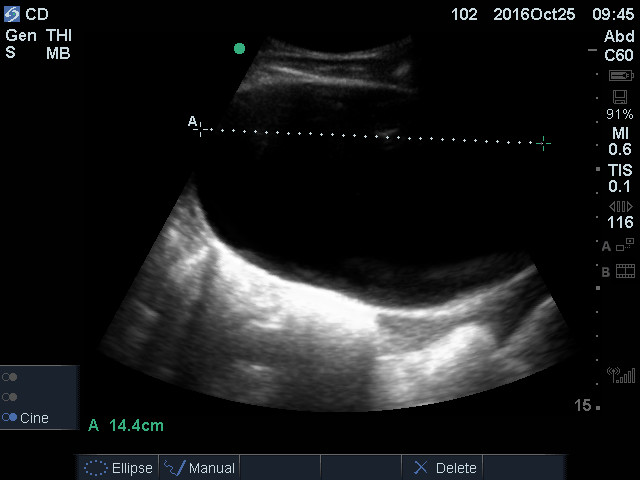
Here is a correctly performed length measurement in the parasagittal view of the distended bladder shown earlier in transverse view.
Next is a distended bladder with an ellipsoid shape in the sagittal plane. The length should have been measured about a cm lower to be in the middle of the bladder, but the distance was about the same over the whole middle range of this bladder.
Store the longitudinal measurement so Venue can calculate the volume and then carefully slide from right to left through the bladder, looking for wall abnormalities.
Bladder volume calculation:
Almost every bladder volume equation begins by multiplying the Width x Depth x Length to get the volume of a cube. The literature agreement stops at this point.
The bladder is infrequently a cube, so a correction factor is usually needed. Every correction factor is based on a geometric shape that might approximate the bladder, and at least eight equations have been used. Each equation makes errors in some patients. Trying to choose the shape of a patient’s bladder and use the equation for that shape makes sense but wasn’t superior in several modestly sized studies. We accept that all the equations may be off by 25% in any patient, but this is acceptable for how we use bladder volume.
There are two primary contenders for the better correction factor. Some ED ultrasound leaders chose a correction factor of 0.75 based on a 1993 study. Another group of non-ED ultrasound physicians decided that many very large bladders resembled a prolate ellipsoid, and the correction factor for this shape was 0.5, so they chose this.
Given that no equation has been better overall, the 0.75 correction factor is reasonable for most moderate-size bladders in the clinic that are roughly triangular in the sagittal view. However, for very large bladders, the 0.5 correction factor will be used because these bladders usually become more ellipsoid. An unusual cuboid bladder requires no correction factor. Venue calculates all three volumes, and the physician decides which to use.
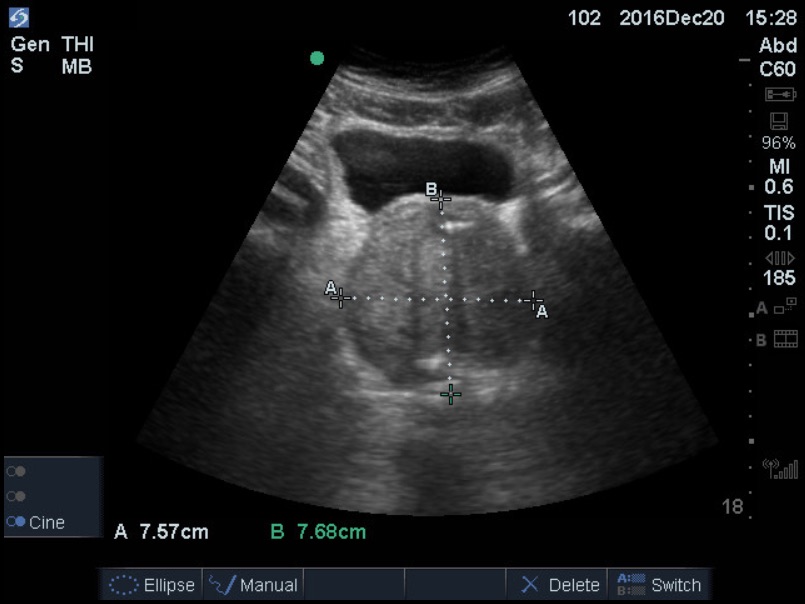
Bladder volume abnormalities: There are two frequent questions in the clinic. “Is there urinary retention?” and “What is the residual urine volume after urination?” The bladder size varies with patient height, but for most normal adults, the urge to urinate begins at about 200 mL of urine volume. Some patients with prostate hypertrophy do not have obstructive symptoms but develop bladder storage dysfunction. They have a strong urge to urinate and can be incontinent when bladder volume is not much over 200. The discomfort with any given amount of urine varies from patient to patient. Acute urinary retention is more uncomfortable than slowly progressive chronic retention. A bladder with > 400 mL of urine indicates urinary retention, voluntary or otherwise. Here is a gigantic bladder that was chronic.
After urination, normal younger adult bladders will have less than 50 mL. In older adults, the detrusor muscle weakens (sometimes from medication) so that typical post-void residuals may be up to 100 mL without concern. Any patient with a bladder question should first be examined with a full bladder (to measure the volume and be able to see the bladder walls and the structures under the bladder), and then the post-void bladder can be re-examined. Important information may be missed when patients are brought only for post-void residual measurement.
Bladder wall abnormalities: The bladder wall can be thickened (> 4 mm) from tumor or inflammation. Below is a longitudinal bladder showing a thickened wall from an infiltrating tumor.
Bladder diverticula can be single or multiple, small or large, but they are additional anechoic structures beyond the typical bladder wall. A visible narrow channel is usually seen between the primary bladder and the diverticulum. Here is a diverticulum from a patient with chronic UTIs and multiple diverticuli.
Stones in the bladder are dependent and hyperechoic with posterior shadowing. Blood clots and tumors can also be imaged along the bladder wall. Blood clots are usually not adhesive to the wall and move with position change. Tumors of the wall will not move. Here is a clinic patient with hematuria. The first clip is the transverse view of the bladder, showing structures on the side wall defying gravity.
Here is the same bladder in the sagittal plane.
These masses did not move with position change and were found to be carcinoma.
However, here is a patient who had only a partly full bladder, and in the sagittal plane, something looked suspicious in the anterior cephalad wall. Transverse views suggested this might be on the left side. Instead of immediately generating a urology consult for cystoscopy, this patient was asked to come back with a full bladder for a better exam, and the abnormality was no longer seen.
Finally, here is a large mass in the bladder that seemed to be coming from the prostate. The patient was very ill, was hospitalized, and was also found to have a brain mass. He died within a week without a definition of the tumor type.
MALE PELVIS
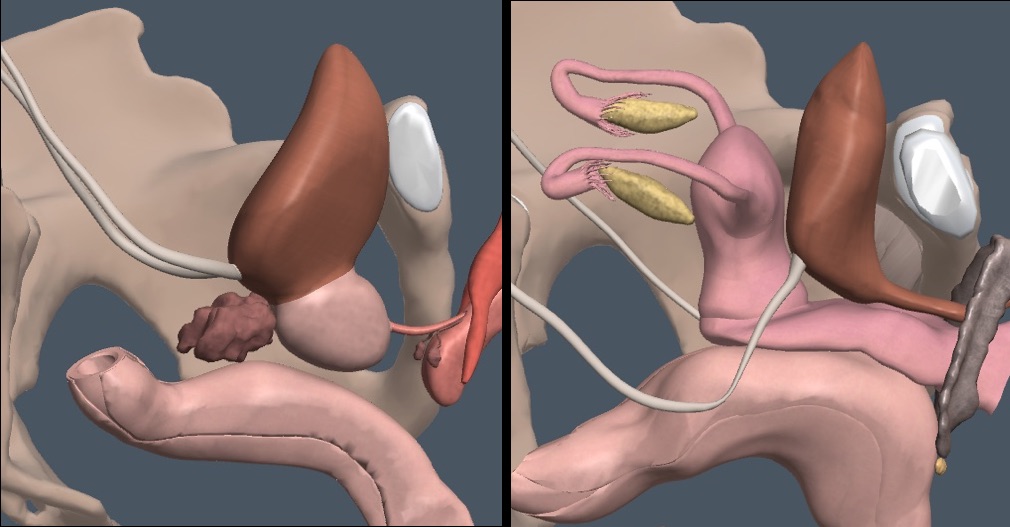
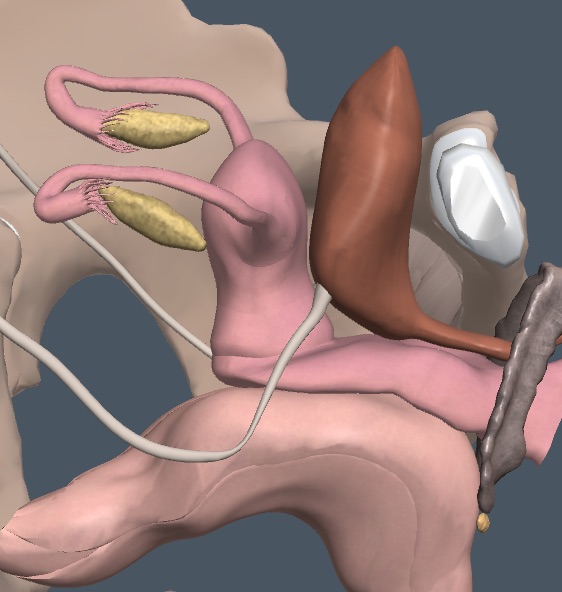
In men, the prostate and seminal vesicles lie posterior and caudal to the bladder and anterior to the rectum.
Transverse view of the Prostate
The probe must be angled caudad of the bladder in the transverse plane to bring the prostate into view. The seminal vesicles may or may not be seen cephalad and lateral to the prostate. We think it is vital to stay near the pubic symphysis and try for as perpendicular a plane through the prostate as possible. A more oblique angle may falsely increase the measurement of the prostate depth.
Imaging the hypoechoic prostate for measurement requires optimizing depth, focus position, gain, and sector width. Posterior acoustic enhancement from a full bladder can over-gain the prostate, requiring TGC adjustment. However, the gain should not be reduced too much. The zone anterior to the hypoechoic glandular tissue contains two capsules and a muscle layer and should be reasonably thick and hyperechoic. Getting this zone correct usually produces a suitable hypoechoic gland for measurement. Accuracy with prostate size estimation is entirely dependent on the quality of the view, which requires high-end equipment and examiner experience.
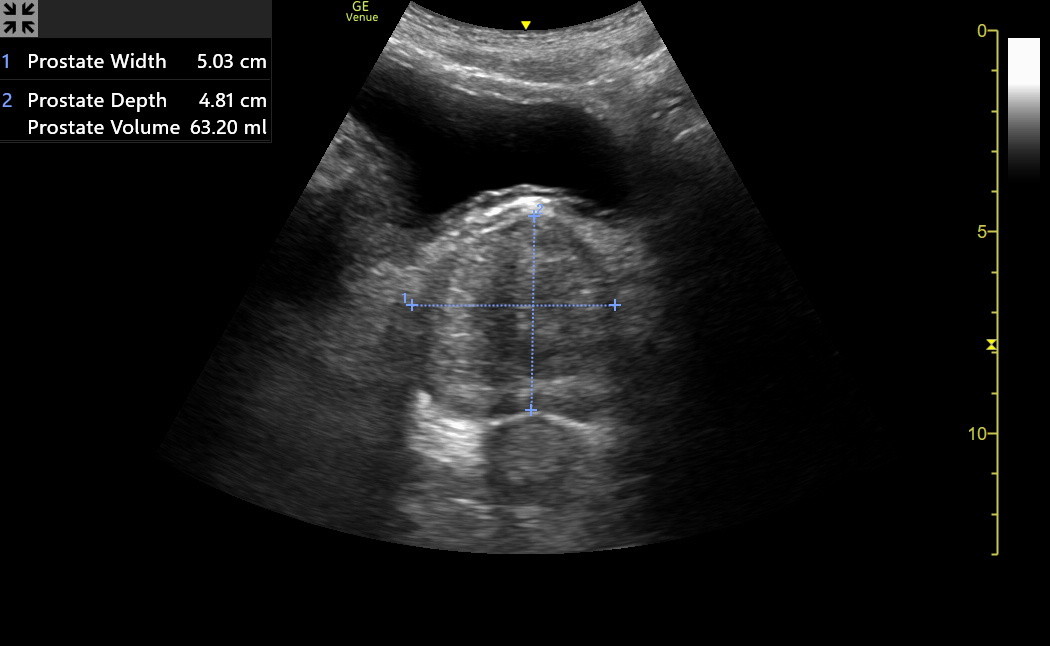
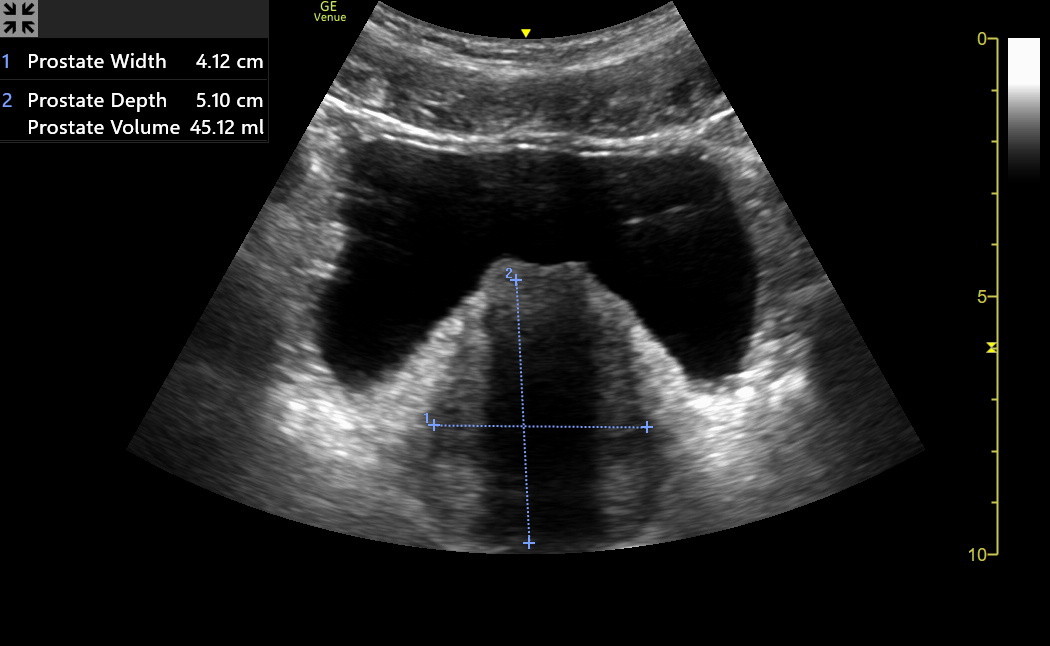
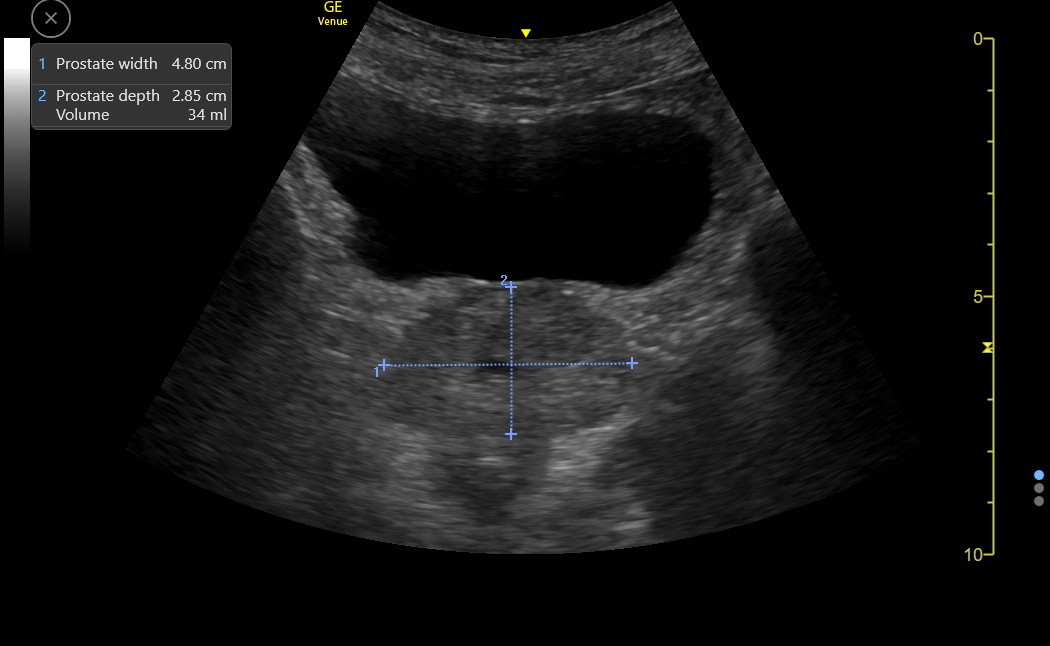
Here is an optimized transverse prostate image. Notice the rectum below the prostate. The width and the depth of the prostate were measured. The width was a few mm too generous on the left side of the image, but this didn’t matter clinically.
Do not include the rectum in the prostate's depth measurement. Fan slowly through the prostate and find a thin, slightly hyperechoic line, which is the fascia separating it from the rectum.
Only the WIDTH and DEPTH of the hypoechoic gland need to be measured. The depth of the prostate is usually more distinct than the width, but unfortunately, the width is the more important measurement. For most patients, overestimating the prostate size may be a worse error than underestimation. Make several measurements of enlarged prostates. Here is a moderately enlarged prostate with measurements. The depth of this prostate was overestimated because the gain was too low, making the anterior hyperechoic zone indistinct. However, this would not have changed the conclusion about this being a moderately enlarged prostate.
Prostate volume calculation
Transabdominal ultrasound sizing of the prostate has agreed well with transrectal ultrasound sizing for clinical purposes, but this depends on the quality of the machine and the physician’s technique.
The formula for a prolate spheroid, which the enlarged prostate resembles, only requires the WIDTH and DEPTH in the transverse plane. This is fortunate because the caudal border of the prostate in the longitudinal plane is often indistinct. The formula is:
Volume = Width2 x Depth x 0.52
The width is the most important measurement, so make this as accurate as possible. The upper normal cutoff for prostate volume in younger men is 25 mL. The Venue will calculate this volume from the measurements. Next is a patient with only mild prostate enlargement (34 mL).
Finally, here is the current ANGMA clinic record for a large prostate with a volume of 220 mL obtained years ago with a SonoSite Edge device.
Prostate compression: Bladder volumes of greater than 400 mL can compress the prostate. In one study, 50 mL prostates were reduced to 41 mL with bladder volumes over 400 mL.
What to do with prostate volume?
Improvement in ultrasound technology is increasing our accuracy with prostate imaging. Nevertheless, categorizing prostates as normal, mildly, moderately, and severely enlarged is better than worrying about differences of single digits in a measurement. Men with symptoms consistent with benign prostatic hyperplasia (BPH) should have some increase in prostate size. The relationship is strong enough that finasteride is only generally recommended for symptomatic men once prostates are over 40 mL. For us, that would be a prostate that is moderately increased. Tamsulosin could be used for symptoms at smaller gland sizes, but be suspicious of a BPH diagnosis with a gland that isn’t over 30 mL.
PSA Density (PSA ng/mL ÷ prostate volume mL): Transabdominal prostate volume was measured with excellent US equipment, and well-trained physicians agreed well with MR obtained prostate volumes in 64 UK men with PSA between 5 and 9 who underwent biopsy for possible cancer. (Pantelidou, et al. PLOS ONE Sep 9, 2022 https://doi.org/10.1371/journal.pone.0274014). In this group, a transabdominal US PSA density > 0.15 ng/mL as a cutoff for biopsy had a 100% sensitivity with a specificity of 98% (the study's small size makes the confidence intervals relatively wide around these estimates).
Venue images can be good enough in some men with modestly elevated PSA that a PSA density less than 0.15 ng/mL can be used to observe the patient for an interval, followed by a repeat PSA density analysis. This would safely delay, or even avoid, referral for likely MR and perhaps a biopsy. A patient with a PSA of 4.0 and a prostate volume of 40 would have a density of 0.10 and could be observed, while a patient with a PSA of 5.0 and a prostate volume of 30 mL would be over the cutoff and need referral. A PSA of 9.0 would need a referral unless the prostate volume were > 60 mL. We need excellent images and several repetitions of the volume measurement to be as accurate as possible when using this approach.
Focal hypoechoic or hyperechoic areas can be seen in a prostate, and these can be infection-related or tumor. Calcifications can accompany hyperplasia or tumors. Ultrasound can’t determine the exact diagnosis of these abnormalities.
Longitudinal male pelvis view
Rotate the probe to the sagittal position and move the depth beyond the prostate until the rectum is seen. Observe the area cephalad of the prostate and posterior to the bladder, where free fluid in the pelvis should be best seen. The sagittal view is better than the transverse view for identifying fluid. As noted above, the semi-upright patient position may improve fluid detection. Here is a patient with fluid in the rectovesicle space. The seminal vesicles were also seen cephalad and lateral of the prostate, but these are in the extraperitoneal space.
Here is a clip from a younger man with an almost invisible prostate who had modest free fluid in the rectovesicle space.
FEMALE PELVIS
Imaging the ovaries, uterus, or vagina well requires a urine-filled bladder. Here is the relevant anatomy.
Caution: IMBUS skill and experience can never be good enough to evaluate a young woman in early pregnancy. Such a patient with pelvic complaints needs an immediate OB or ED visit. Enlarged and heterogenous uteri from fibroids are common in older women, and distinguishing benign from malignant is difficult. Formal transvaginal and transabdominal ultrasound and gynecology referral are needed in symptomatic women. Finally, enlarged and cystic ovarian structures in post-menopausal women would be suspicious findings requiring formal imaging and gynecology follow-up. Follicular cysts in menstruating women may be up to 2.5 cm in width, and these could be followed in the clinic for resolution.
Transverse view
Here is a transverse view of a nulligravida patient with a full bladder. The probe was angled cephalad through the bladder to view the uterus, which contained an IUD in the center. The patient’s right ovary is in view.
Multigravida patients will have larger uteri, and a normal uterus can be more lateral than central. The ovaries are usually lateral near the iliac vessels but are not always easy to see. However, if the following image were obtained in a post-menopausal woman, there would be a cancer concern. The uterus is heterogenous and enlarged, with a 2.5 cm cyst in the right ovary.
Longitudinal view
Here is the longitudinal view of a normal multigravida, premenopausal, non-pregnant woman. The vagina is immediately posterior to the bladder on the right side of the screen. The rectum is below the vagina. The uterus is just below the bladder on the left side of the screen. The uterine stripe can be seen intermittently in the center of the uterus. The cervix is at the end of the uterine stripe.
The critical rectouterine space that might contain small amounts of intra-peritoneal fluid is shown in the following image (arrow pointing to the fluid).
 The ovaries can usually be seen by sliding transversely across the area. Here is the previous premenopausal patient, with the probe moved laterally to show the normal left ovary with several small cysts. The briefly seen tubular structure is an iliac vessel.
The ovaries can usually be seen by sliding transversely across the area. Here is the previous premenopausal patient, with the probe moved laterally to show the normal left ovary with several small cysts. The briefly seen tubular structure is an iliac vessel.
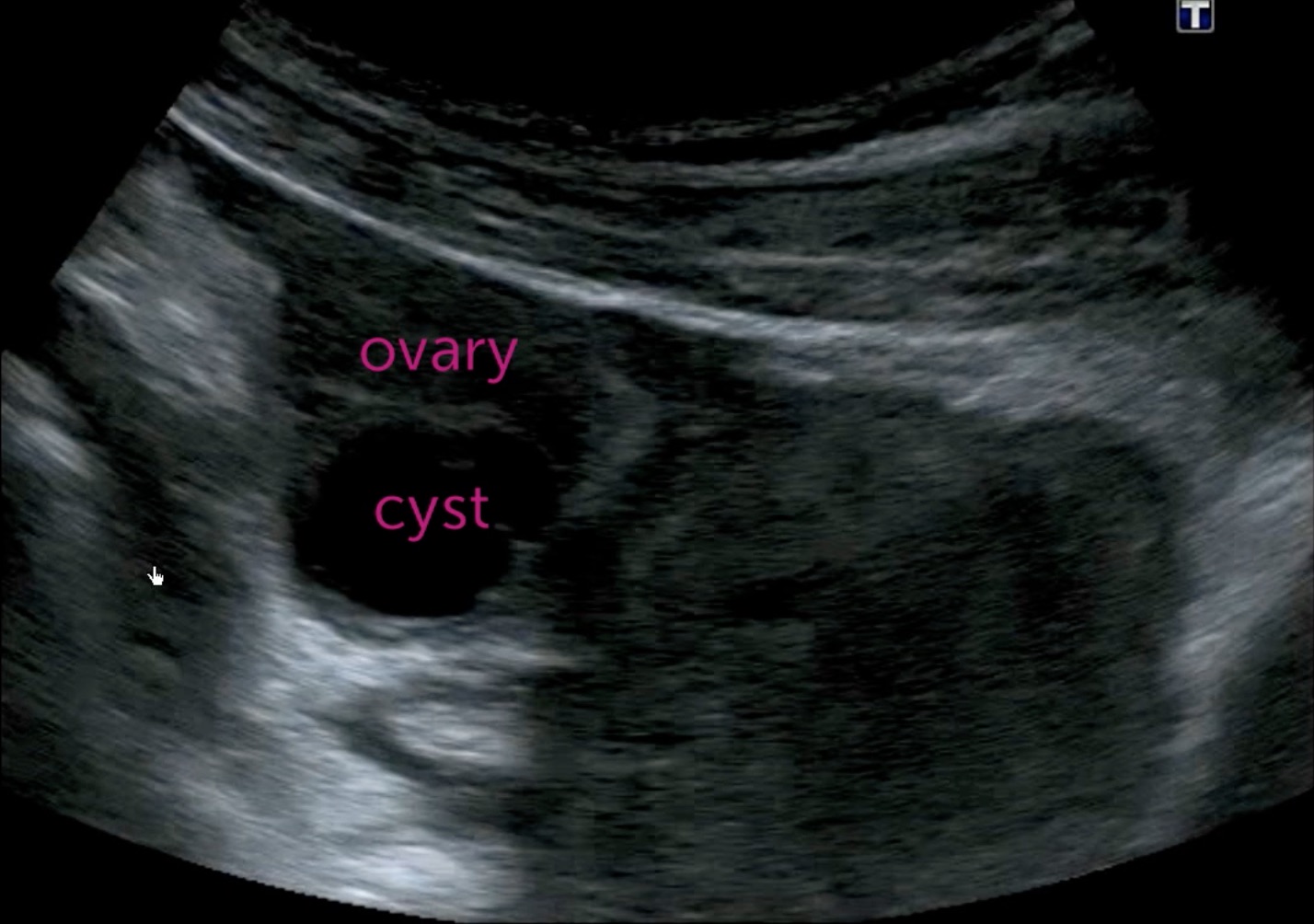
Next is the right ovary in the same patient, showing a dominant cyst about 2 cm long with several smaller cysts. The iliac artery and vein are anterior to the ovary. These cysts can be a normal part of the menstrual cycle and usually resolve spontaneously without symptoms. No follow-up would be needed in a premenopausal woman who was not pregnant unless there were symptoms. This same appearance in a postmenopausal woman could still be normal but would warrant short interval follow-up to see regression and not growth.