Liver Region Imaging
The IMBUS-Advanced exam of the liver region is more than just looking at the gallbladder and bile ducts.
A clinic IMBUS exam of the liver region is most frequently needed for patients with subacute epigastric or right upper quadrant discomfort that suggests gallbladder (GB) disease. This exam may also be helpful as part of the exam of systemically ill patients and patients with lab abnormalities suggesting hepatobiliary disease. Thus, it is essential to learn to do a comprehensive but efficient exam that includes the liver parenchyma, hepatic veins (HV), portal veins (PV), bile ducts, and GB. This chapter will discuss anatomy, technique, and normal findings, while the next chapter will cover abnormal findings in the liver region.
The liver region exam varies from patient to patient depending on the location of the transverse colon, the amount of adipose tissue, and when the patient last ate. To address these variables, an IMBUS-advanced physician needs to know several approaches to the exam. Whatever the method, knowledge of critical anatomic details is essential for a good and efficient
LIVER ANATOMY
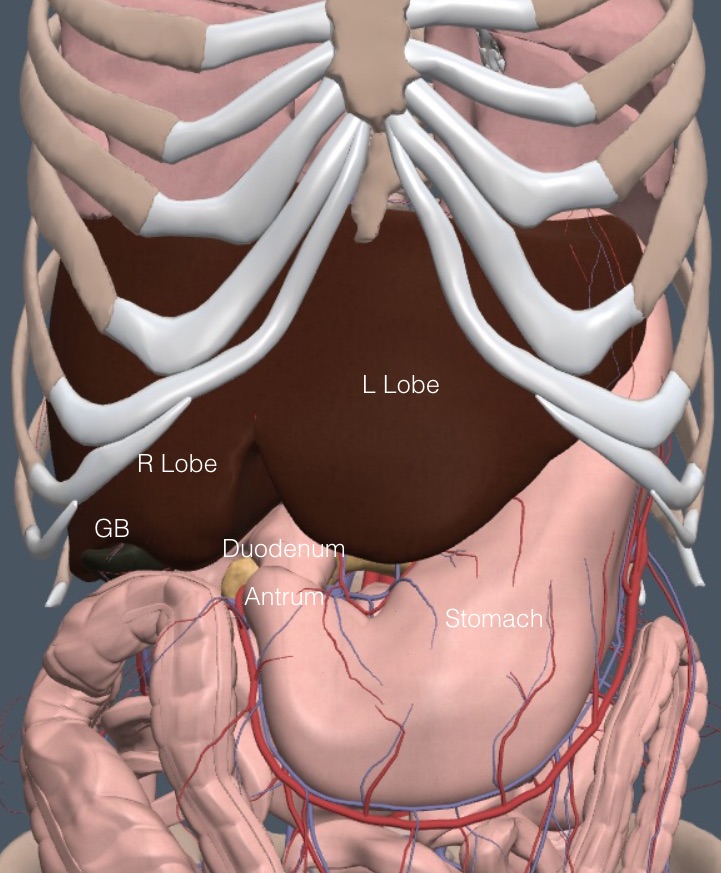
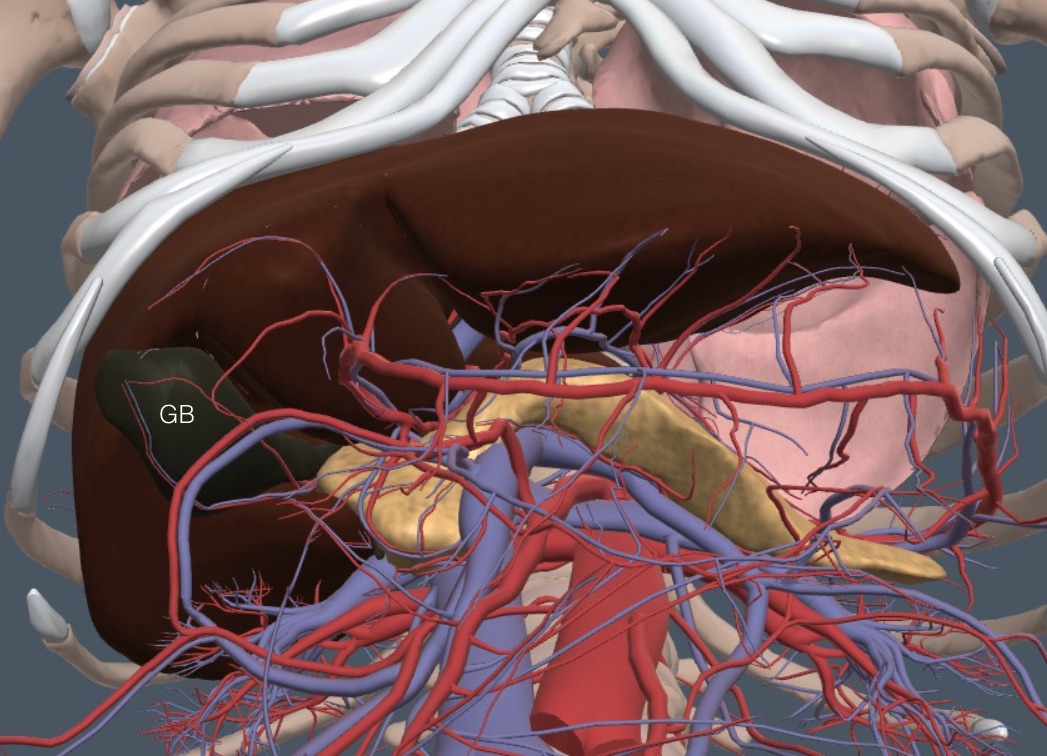
With anterior structures removed, the following frontal anatomy view suggests that examining the liver and GB should be easy. Yet, when muscles, connective tissue, adipose tissue, and digestive tract contents are added, the exam becomes more difficult.
The liver is divided into functional segments based on the HV and PV divisions. The concept is simple, and we don’t need to know the segments by number. Three HVs drain cephalad to the IVC. The middle HV (MHV) divides the liver into the right and left lobes. The right and left HV (RHV, LHV) divide each main lobe in half to create longitudinal quarters. This is shown schematically in the following diagram with the HVs in blue.
The longitudinal quarters are divided in the transverse plane by the right and left PV (RPV, LPV), shown in purple in the diagram above. Ignoring the numbering system, it is enough for us to know we are viewing the “upper, medial portion of the right lobe.”
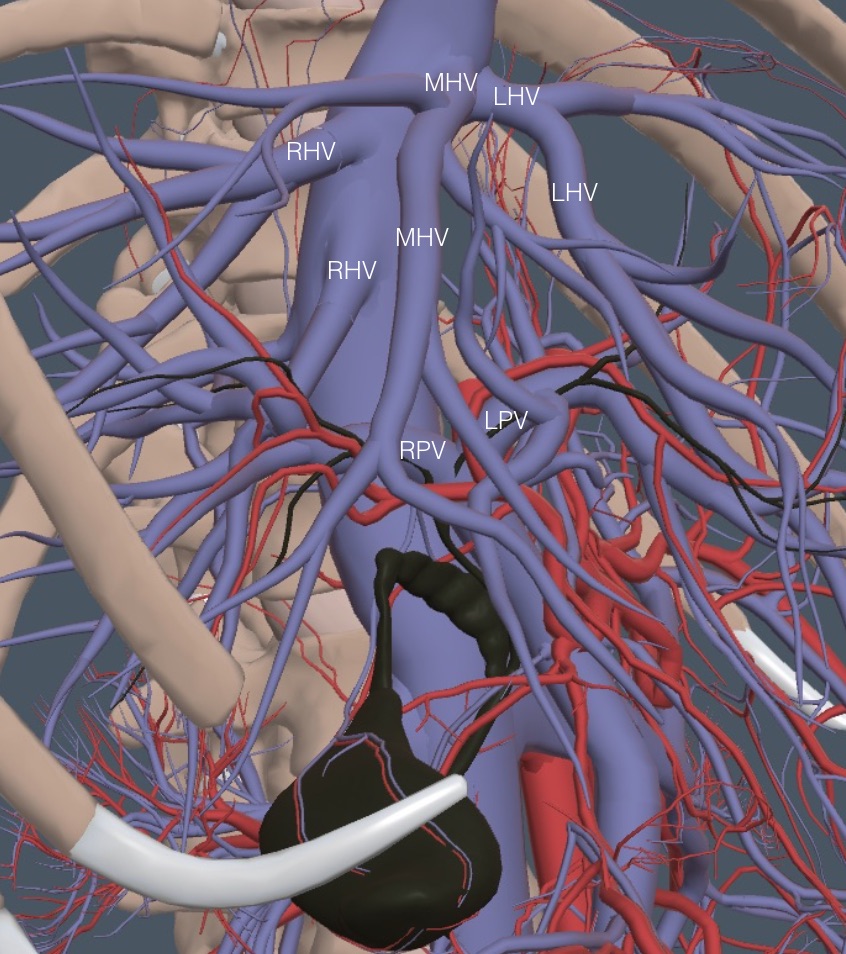
The following view shows more detail of the vein anatomy, as seen with the body turned about halfway toward the left lateral decubitus position.
Notice that the RHV may be two separate veins draining into the IVC. Thus, the HVs are often seen one or two at a time unless a particular oblique view is obtained, as in the following clip. Notice that the HVs have thin walls that are minimally hyperechoic.
In contrast, intra-hepatic portal veins have hyperechoic walls. The following clip shows a left portal vein with hyperechoic walls.
Porta hepatis:
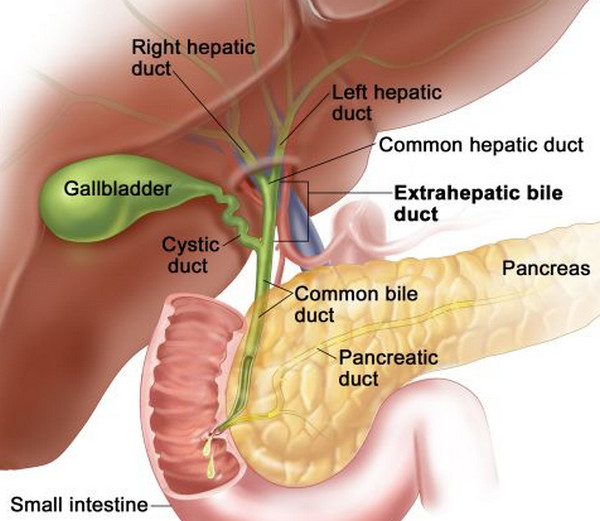
The porta hepatis (PH) is a fissure on the inferior surface of the liver through which the neurovascular bundle and the bile ducts enter and exit. At the PH level, separate right and left HDs join to form the common HD.
A little further caudad the common HD is joined by the cystic duct (rarely seen with IMBUS) to form the CBD. The CBD then runs vertically through the medial margin of the head of the pancreas into the duodenum.
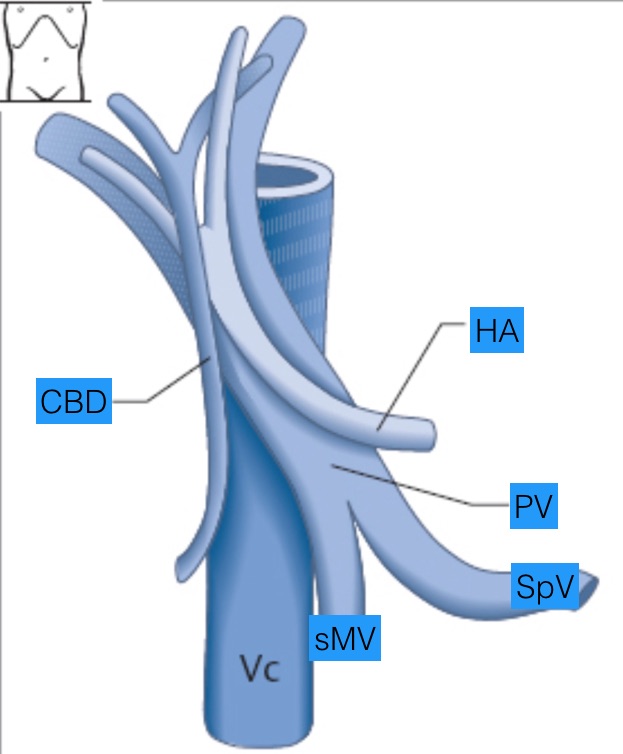
The following frontal view diagram emphasizes the crucial relationships in this extra-hepatic region. The IVC is always the most posterior and the largest vessel. The PV runs oblique and anterior to the IVC. The distal CBD is anterior to the PV and runs mainly parallel to the lateral edge of the IVC. At the same time, the hepatic artery is just posterior to the CBD, parallel to the PV. Near the PH, the common HD more closely parallels the orientation of the PV, but it is still anterior to the PV and the HA.
Gallbladder and bile ducts:
The GB, cystic duct, HD, and CBD have anatomic variants that won’t be detailed here. However, the GB fundus always lies on the inferior surface of the liver. Below is the most common anatomy, with a view looking up at the undersurface of the liver. The GB fundus peeks out below the inferior border of the right liver lobe. The GB body and neck then run posteriorly and medially on the inferior liver surface toward the pancreas and duodenum.
HOW TO IMAGE
The curvilinear probe is used with an abdominal preset. The standard radiology ultrasound exam includes a parasagittal and transverse subcostal sweep on a patient who has been fasting for 6 hours. This subcostal approach is traditionally performed using the left lateral decubitus patient position and patient inhalation to help move the liver into better view.
Many clinic patients have cephalad transverse colons and thick adipose layers, producing suboptimal subcostal windows. In addition, many are not fasting. We are describing the subcostal approach first but emphasize that the intercostal approach described second is needed for many of our patients. Patient exhalation will help the intercostal approach because it moves the lung out of view and elevates the liver above the costal margin.
With any imaging approach, a short halt in breathing is essential for viewing critical structures. Don’t try to evaluate everything in constant motion.
Here are the overall things to evaluate:
- Form and overall size of the liver
- Capsular contour (smooth, coarse, lobulated)
- Liver echogenicity compared to the kidney parenchyma
- Homogeneity of the liver parenchyma: masses, collections of things
- HV size and patency
- PV size and patency
- GB size and structure
- Bile duct size
Liver Size:
Expert groups don’t agree on a particular measurement of liver size because the organ varies in shape and depends on the patient's size. As a European US course book said, “Liver size measurement has no impact in daily routine because there is no reliable and reproducible ultrasound method established so far.” There is agreement that a liver extending caudad of the right kidney is enlarged if it isn’t just a downward elongation of an isolated lateral portion of the right lobe of the liver (Riedel variant). The caudad extension of the liver can be seen with either subcostal or intercostal views through the right liver lobe. Here is a clip of a parasagittal subcostal view showing an extension of the liver below the right kidney. However, this extension was isolated to the lateral right lobe and was a Riedel variant.
Another marker of hepatomegaly is a rounded inferior edge of the left liver lobe in a parasagittal view in the left upper epigastrium instead of the normal acute angle. The following clip shows a normal acute angle.
THE SUBCOSTAL APPROACH
Use held patient inhalation to bring the liver caudad for better viewing during the subcostal approach.
Step 1: Left epigastric
Get a parasagittal probe position over the left liver lobe. Evaluate the smoothness of the liver contour and whether the edge of the liver looks rounder than usual.
Then, rotate to a transverse probe position over the left lobe of the liver and fan through the parenchyma, including the left portal vein. Here is the hand and probe position.
Viewing the most distal common bile duct: this is only possible in thinner patients without duodenal gas shadows, which means it is rare in our clinic patients but fun and rewarding when it happens.
Method: slide the transverse transducer caudad in the mid-epigastrium to find the splenic vein, which leads to the PV. In the following patient, the physician found the splenic vein and showed it flowing into the origin of the PV.
The PV and the IVC are the guides to the most distal CBD, which runs anterior to the PV but mainly parallel to the right edge of the IVC. The distal CBD enters the head of the pancreas at the level of the PV origin.
Once the origin of the PV is found, slide the probe so the IVC and PV are more centered. Then, rotate slowly toward 12:00, staying at the lateral edge of the IVC. Watch for the CBD to appear anterior to the PV. Here is the result of that positioning in the patient just above, showing the distal CBD enteringIn the following clip, the probe rotation toward 12:00 and slide to the lateral edge of the IVC was repeated a little higher in the epigastrium of the same patient, giving a slightly different view of the vessels and CBD. The IVC is mostly in long-axis, while the PV is oblique.
Normal distal CBD diameter is about 1 mm per decade of life after about age 40 but can be a little larger in post-cholecystectomy patients. Normal CBDs are thin by eyeball and don’t need to be measured after a modest amount of training. An enlarged CBD immediately grabs attention because it is half or more the diameter of a normal PV. In the patient shown above, the PV had a diameter of about 1.0 cm, and the CBD was less than half as wide, so it was normal.
Step 2: Transverse subcostal sweep
Move the probe obliquely underneath the beginning of the right costal margin. The indicator should point toward the physician. Fan as anterior as possible to see the diaphragm and then begin a slow posterior fan through the liver. If the view is medial enough, the HVs will usually appear anteriorly as they join the IVC. The HVs may enter at slightly different locations, as shown at the beginning of this chapter.
An obliquely or horizontally oriented right PV should appear fanning a little posterior from the HV. This has been described as looking like an animal jumping over the IVC toward the patient’s left. Most of the animal is the long-axis right PV with its hyperechoic walls. Because this view is higher in the liver, the thinner HD is the bile duct to be seen, and it runs right on top of the PV. Here is a PV looking like a dog jumping over the IVC. A thin HD runs along the back of the dog.
The GB will often appear while fanning posterior from the PV, seeming to come out of the animal's tail. The cut through the GB depends on how a patient’s GB lies on the inferior liver surface. Gallstones can be observed during the posterior fan, and GB wall thickness (normal < 5 mm) may be measured at the anterior wall that is interfacing with the liver. However, a contracted GB is not always easy to see. Here is a clip of a partially contracted GB during this posterior fan. The patient had eaten a lot of fat about 1.5 hours before the exam.
Step 3: The long-axis GB
Slide one probe width at a time to the patient’s right underneath the right costal margin, fanning anterior and posterior through the liver parenchyma. At some point, the fundus of the GB should appear at the inferior liver margin. Here is a typical subcostal probe position where the GB fundus might be seen.
When the GB is glimpsed, rotate the probe slowly clockwise (indicator moving anterior) until the best GB long axis is found. Below is a fasting patient with a GB in the long axis. The PV was in short-axis in this patient, forming the classic “exclamation point.” The aorta and IVC are to the right below the GB, with the IVC partially obscured by the shadow from duodenal contents.
The first view of the GB must be deep enough to see any shadows coming from stones, particularly in the neck of the GB, where stones can hide. Fan through the long axis GB, which can be up to 10 cm in length and 4 cm in width in the fasting state.
Bile ducts: The variability of the GB position means that many patients won’t have an exclamation point appearance of the GB and PV. It doesn’t matter. Focus on the PV and the IVC. Rotate the indicator clockwise while fanning to the lateral edge of the IVC. The bile duct will appear anterior to the PV. If necessary, check Color/Power Doppler to see flow in the PV and IVC but not in the bile duct.
The following clip is from the patient above with the exclamation point GB/PV. The probe was rotated clockwise until the IVC was mostly long-axis. The PV was partly long-axis, and the GB was fading out of view. When the probe was fanned to the lateral edge of the IVC, a 3 mm bile duct was visualized.
Contracted GB versus duodenum: Since most clinic patients have not fasted for six hours, contracted GBs are common, and the duodenum can be mistaken for GB. The next subcostal view near the right liver lobe showed a structure that a novice could mistake for a GB filled with small stones because of a posterior shadow. However, notice that the outer wall of this structure is HYPOechoic, and the shadow is “dirty.” This is the duodenum.
In contrast, the following is a long-axis view of a partially contracted, otherwise normal GB, showing a HYPERECHOIC outer wall, a middle hypoechoic layer, and an inner hyperechoic layer, distinguishing it from the duodenum. In a contracted GB, the hypoechoic middle layer is not edema in the wall. Do not measure the wall thickness on a contracted GB.
The rest of the right liver lobe: After finishing the GB and bile duct exam, continue sliding transversely under the rest of the right costal margin, fanning anterior and posterior through liver parenchyma. Past the mid-clavicular line, the kidney should appear posteriorly. If the liver is large, it would extend below the kidney. The following is a subcostal view of normal liver and kidney. This can be an excellent view for assessing the echogenicity of the liver next to the cortex of the kidney. Fanning further caudad can determine if the liver extends beyond the kidney.
THE INTERCOSTAL APPROACH
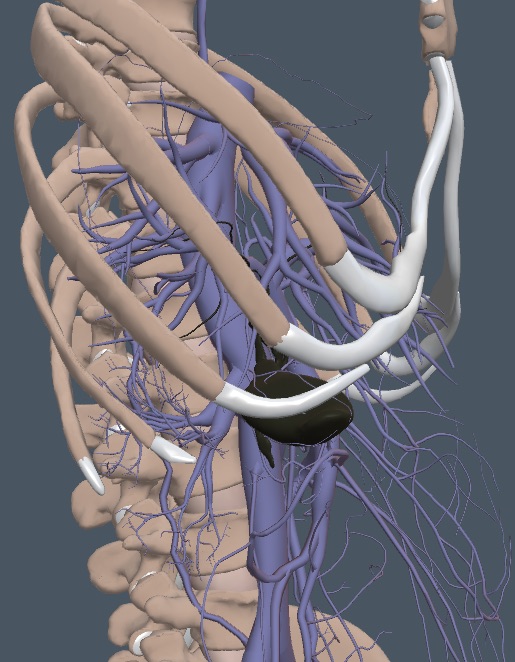
The following image shows the open intercostal spaces caudad of the lungs but cephalad of colon. All this space is available to view the liver region. The left lateral decubitus position is best for physician hand and arm placement.
Wherever the probe is placed in the intercostal spaces, the physician must know how the GB, PV, HV, IVC, and bile ducts are oriented. Here is how the physician typically views the GB when the patient is in the left lateral decubitus position.
Intercostal method:
Deep inspiration is NOT an advantage because the lung should be kept out of the lower intercostal spaces. Have the patient breathe quietly and periodically hold an exhalation for best viewing. All the views of structures discussed with the subcostal approach can be reproduced in the intercostal spaces if the physician focuses on the anatomical relationships. Begin with an intercostal space at about the right mid-axillary line. Slide the probe between the lung border and the bowel gas to find the best window and rotate to be completely intercostal. Push modestly into the space and fan anterior to posterior. Have the patient exhale and stop breathing to examine a still liver.
Continue to move toward the patient’s midline one interspace at a time. Find the window between lung and bowel gas and fan anterior to posterior in each interspace. This stepwise approach ensures that the liver is well visualized and the gallbladder and bile ducts are seen from different angles. The intercostal spaces toward the midline become more horizontal.
Here is an intercostal view of a GB as it was first seen.
The probe was then rotated to create a long-axis IVC and a short-axis PV. A mostly long-axis GB resulted. A normal bile duct is present just anterior to the PV. Decreased depth could have been used if more bile duct detail had been needed, but the duct was much smaller than the diameter of the PV, so it was normal.
PORTAL VEIN DOPPLER
CVP versus organ-level venous congestion: The CVP reflects the right atrial pressure, which helps determine whether a patient is fluid-tolerant. However, it doesn’t tell us whether a patient’s cardiac output will increase with volume challenge. The CVP also does not identify intra-abdominal, organ-level venous congestion, which causes organ dysfunction in some patients.
CVP can be dissociated from organ-level venous congestion because the latter depends not only on RAP but also on pleural space pathology, intraabdominal pressure, osmotic/oncotic pressures, and possibly a few other factors. Clinical trials are investigating how to treat patients with kidney dysfunction and organ-level venous congestion despite non-elevated CVP.
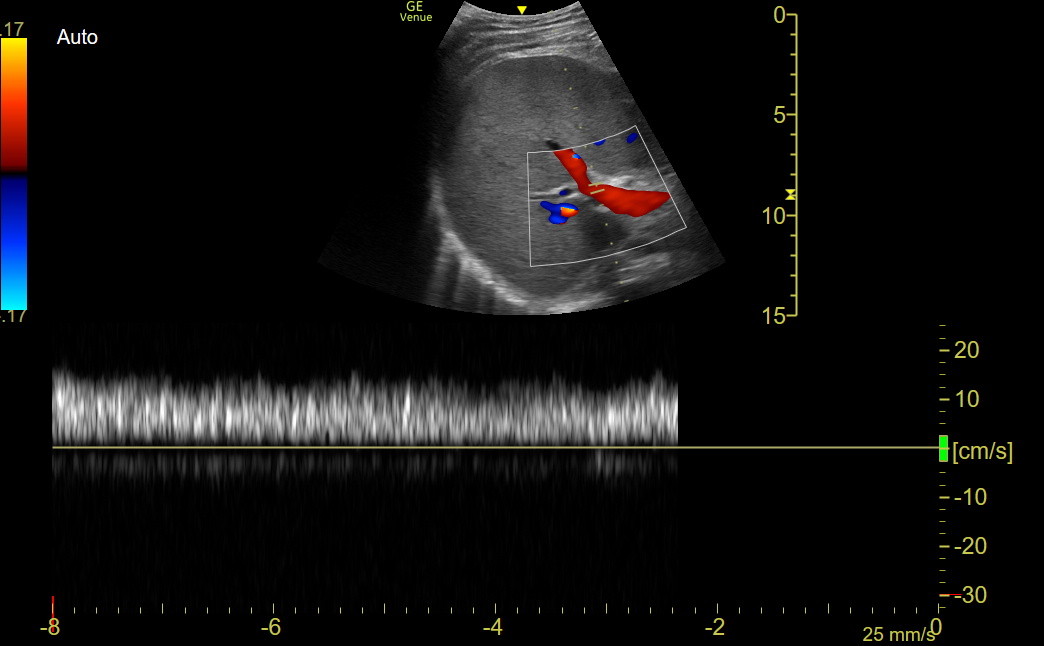
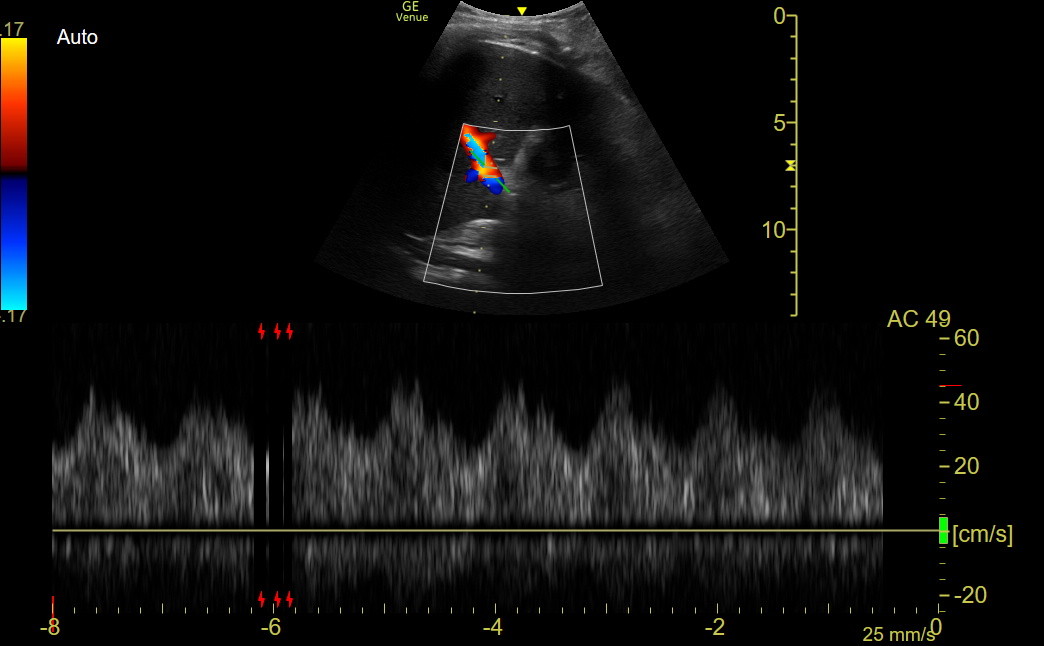
A group of primarily critical-care-oriented physicians developed a VeXus exam (venous excess by ultrasound). This exam used PW flow patterns of the hepatic, renal, and portal veins to identify organ-level venous congestion. The PV pattern is the easiest to obtain and interpret and remains useful with severe tricuspid regurgitation. Obtain a long-axis right PV view in a mid-clavicular line intercostal space. Use Color to find the view with good flow during held exhalation and place the PW gate parallel to flow. Get the tracing during the next held patient exhalation to eliminate respiratory variation. The normal pattern is monophasic or minimally undulating, as in the following Venue image.
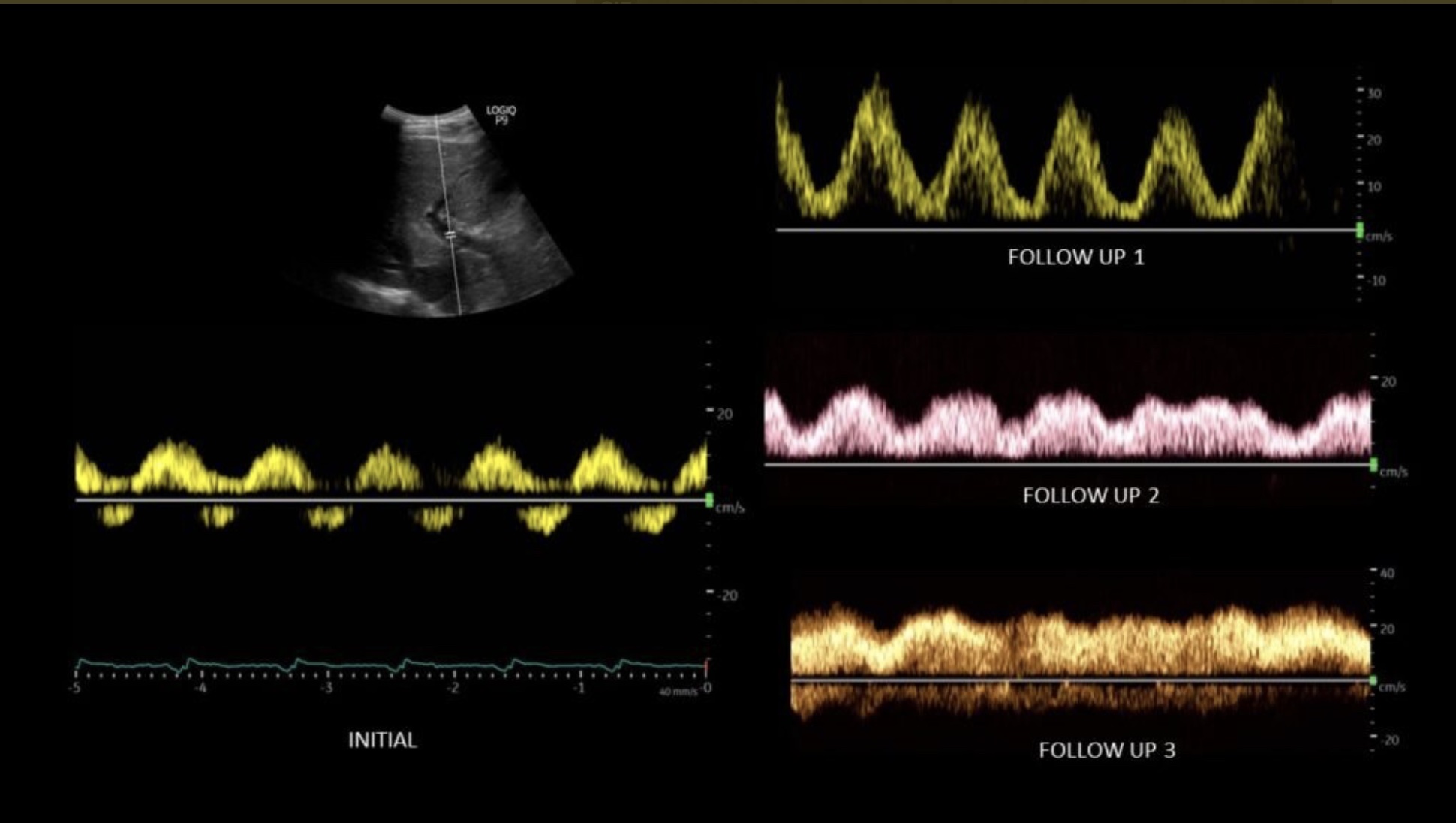
As organ venous pressure increases, the PV flow becomes pulsatile, as shown in the following case from Twitter. The patient had kidney injury, strongly elevated right atrial pressure, and was treated with diuresis. The initial image showed biphasic flow with even some reversal of flow. The first follow-up showed a conversion to just pulsatile flow, and subsequently, the pulsatility diminished to mostly monophasic flow. The kidney function also improved. The PV flow pattern responds relatively quickly to RAP changes.
Next is a tracing from one of our clinic patients with edema and an elevated TV gradient; the biphasic pattern was distinct.
PV flow in portal hypertension: The PW pattern in portal hypertension is undulating to biphasic, as in organ-level venous congestion, but the flow velocity is reduced. PV velocities of about 0.15-0.20 m/sec are seen in normal patients and don’t seem to decrease as organ-level congestion worsens. In the patient described above, the velocity peak was 0.3 when the patient was decompensated and returned to about 0.2 when improved. Patients with portal hypertension are noted to have velocities of 0.10 or less.
HV thrombosis and PV thrombosis: HV thrombosis (Budd Chiari syndrome) is rare, manifesting as an acute liver injury with signs of acute portal hypertension. IMBUS can image the HV, apply Color and PW, and get firm evidence of the absence of HV flow. PV PW is also likely abnormal when HVs are thrombosed. PV thrombosis causes a decrease or lack of flow in the PV.