Nasal Sinus
How to evaluate the maxillary sinus with ultrasound for the presence of fluid
IMBUS of the maxillary sinus is a basic exam, but it exemplifies improved diagnostic accuracy, reduced cost, and improved patient satisfaction.
Traditional outpatient diagnosis of acute rhinosinusitis frequently results in the overuse of antibiotics. IMBUS of the maxillary and frontal sinuses is specific for clinically meaningful fluid but may miss subtle soft-tissue abnormalities that are usually clinically unimportant. The ethmoid sinuses are challenging to image and rarely abnormal in isolation. Beyond initial experience, the frontal sinus only needs to be examined when the maxillary sinus is normal and the patient complains of forehead discomfort. The absence of maxillary and frontal sinus fluid is a compelling reason to avoid antibiotics in most patients. A negative ultrasound can also be reassuring to patients. However, a patient with fever and severe symptoms suggestive of sinusitis but no maxillary or frontal fluid may need empiric antibiotics or a CT scan to look for isolated ethmoid or sphenoid sinusitis. A few published studies, including the ANGMA clinic experience (S. Med J. 2018;111:411-417), indicate that ultrasound can reduce antibiotic use for sinusitis. Only about ¼ of the ANGMA clinic patients with the possibility of sinusitis have fluid in the maxillary or frontal sinus. The presence of fluid does NOT differentiate between viral and bacterial disease, so the final antibiotic decision requires the integration of ultrasound with the rest of the patient’s clinical findings. However, the more fluid, the more likely the infection will be bacterial. The patient needs to be upright for the exam, and we think the standing position is more efficient and ergonomically better for the physician.
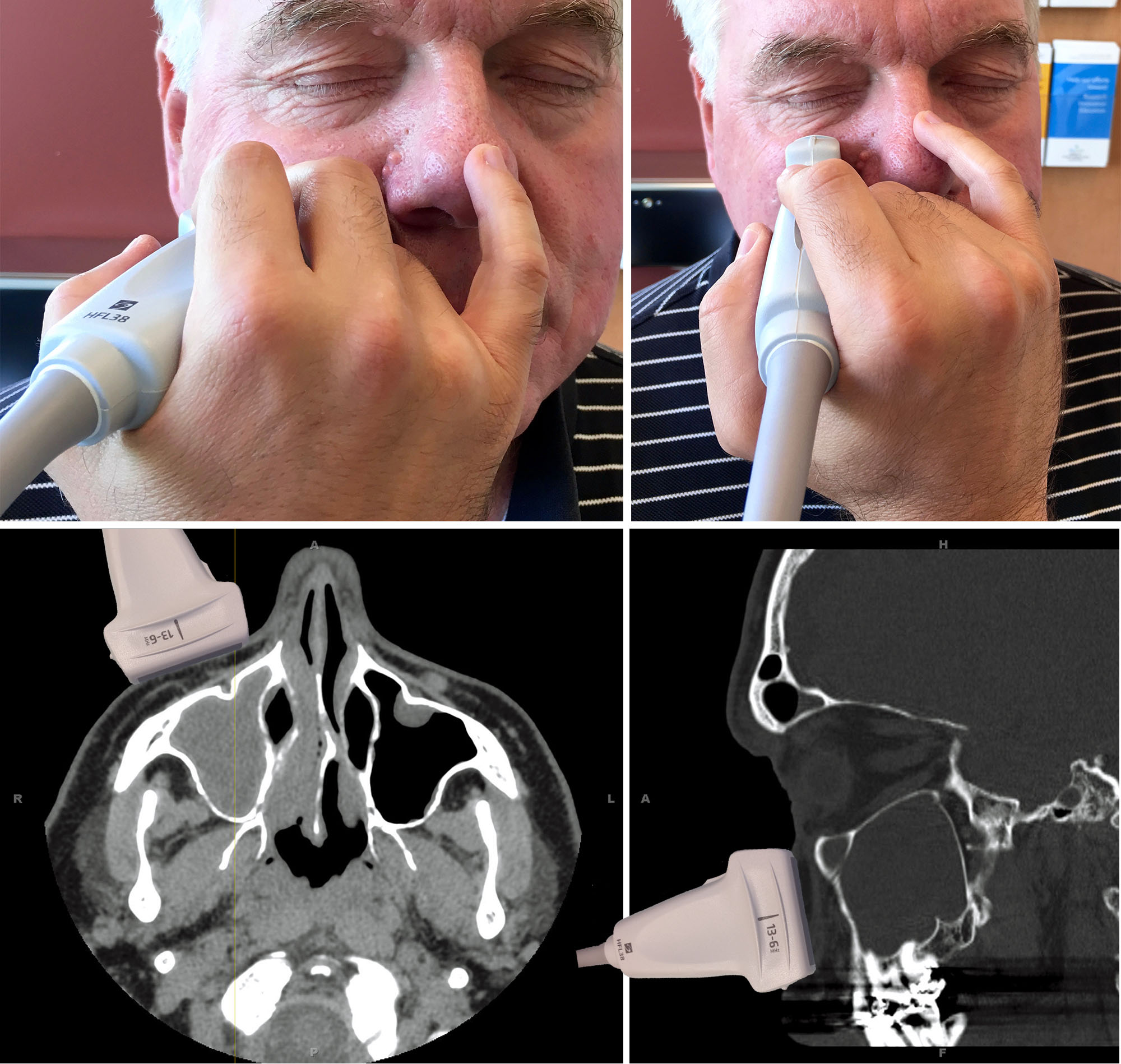
The linear probe is used with musculoskeletal optimization. Our Sinus preset depth is 6 cm. On the patient’s right side, a top and bottom grip is used for the transverse view, anchoring the little finger on the nose. The transverse view begins at the bottom of the nose, rocking a bit laterally so the probe cord moves toward the right ear. The maxillary sinus does not extend laterally beyond the corner of the eye. The probe must be perpendicular to the front wall of the sinus to achieve a distinct, horizontal, hyperechoic anterior wall. The parasagittal view centers on the pupil, rocking the probe slightly down so the probe cord moves toward the chest. Fluid always appears first at the caudal aspect of the sinus. Below are the probe positions with CT correlates.
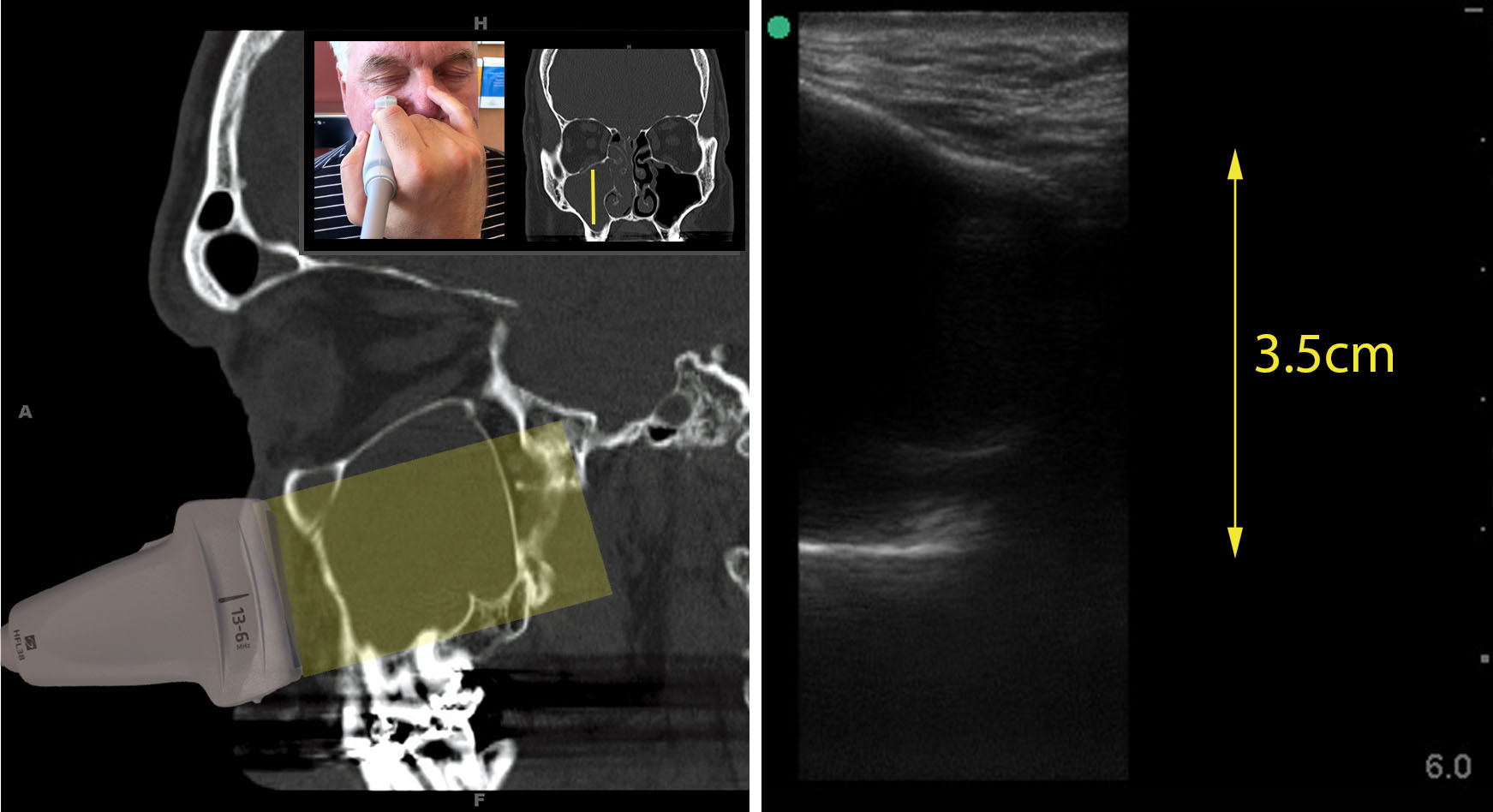
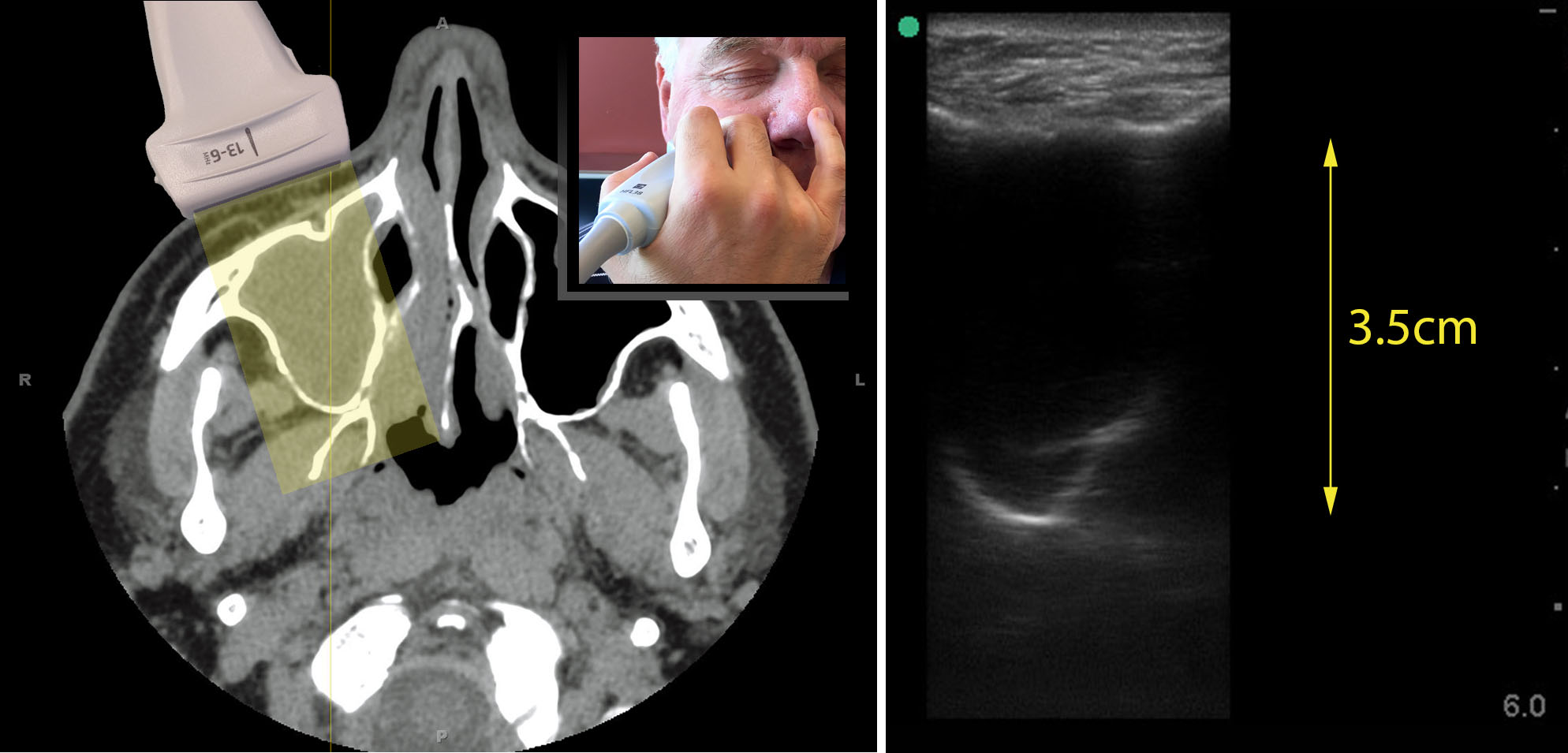
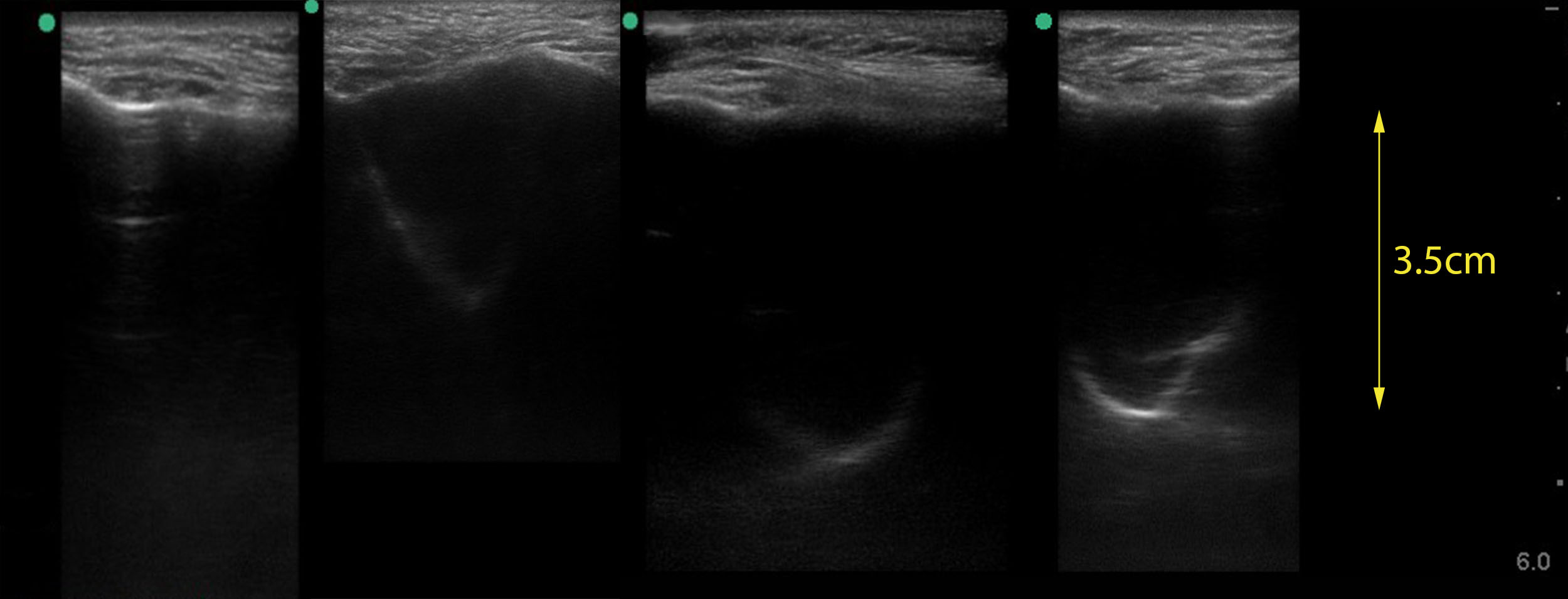
Below is a combination image showing the transverse views of a fully opacified right maxillary sinus with the CT scan on the left and the IMBUS on the right. The “V”- or “U”-shaped back wall is distinctive in the transverse view. In our experience, the back wall is 2.5–3.75 cm from the front wall in adults, depending on body size.
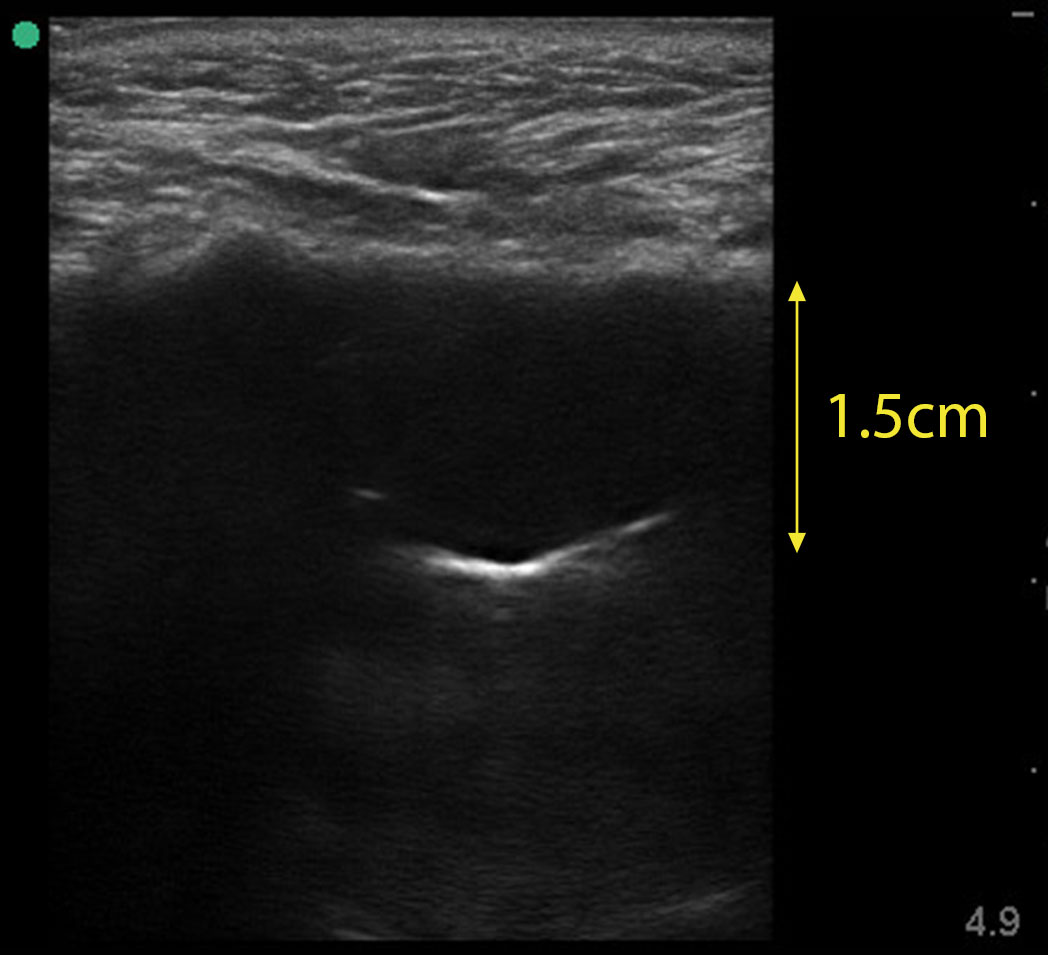
Sinus retention cysts are occasionally seen and are distinguished from free fluid in the sinus by noting that the echogenic back wall is not U/V shaped in transverse and is much shallower; in this case, it is only 1.5 cm from the front wall. These cysts indicate chronic sinus conditions (allergic or infectious) but don’t support acute sinusitis.
Below is the parasagittal view of an abnormal maxillary sinus, which is not as distinctive as the transverse view because a straight echogenic line for the back wall is seen. However, the posterior wall line length corresponds to how high up the sinus the fluid extends. Note that the back wall is not parallel to the front wall of the sinus, helping differentiate it from a reverberation artifact in an air-filled sinus. Experienced physicians often perform the parasagittal view only when the transverse view is equivocal.
For the left maxillary sinus, the transverse hand position on the probe changes to a medial/lateral grip with the little finger anchoring on the cheek.

Below are transverse views of normal left maxillary sinuses. Only the front wall with minimal reverberation artifact may be seen (upper left), but reverberation artifact may be more prominent (upper right, lower left). A mirror image with a single reverberation artifact (bottom right) can look like marked thickening of the mucosa or the posterior wall of the sinus. However, it is not deep enough (1.4 cm from the front sinus wall) to be the posterior wall of the sinus.

Below is the spectrum of transverse maxillary sinus IMBUS findings with normal on the left and strongly positive on the right. The middle two images show weakly positive results with smaller amounts of fluid. The back wall is fainter, and only part of it may show. Depending on the rest of the clinical information, this may lead to different treatment decisions than strongly positive results.
FRONTAL SINUS: This sinus is about 2 cm deep, so the depth setting should be reduced to about 3 cm for the exam. Use a transverse probe at the eyebrow level to examine the frontal sinus. It is not a wide sinus, so you only need to slide between the patient’s pupils. Keep the probe horizontal, or the orbit may be viewed and suggest fluid. Hyperechoic posterior wall signals are curvilinear when fluid is present but not U/V shaped. Here is a young woman with pain under her medial eyebrow. Fluid is present, and there is a reverberation artifact below the back wall of the sinus. Her maxillary sinuses were normal.