Internal Jugular Vein & Inferior Vena Cava
Understanding the physiology and ultrasound evaluation of the IJV and IVC
Right atrial pressure (RAP) and systemic venous pressure assessment are helpful, and this chapter discusses using the internal jugular vein (IJV) and inferior vena cava (IVC) to infer RAP. The Atria chapter describes using Doppler E/e’ to assess RAP, and the Liver chapter will use Doppler of the portal vein to assess systemic venous pressure.
INTERNAL JUGULAR VEIN (IJV)
We assess this vein in sitting patients when elevated right atrial pressure (RAP) is a clinical concern. However, we do not evaluate the IJV as part of a screening heart exam. The assessment is of little use when the suspicion is low RAP.
KEEP IT SIMPLE: The details of assessing the IJV and jugular venous pressure (JVP) are not discussed here because they matter to very few physicians. A simple approach is good enough for most patients.
1. The overall approach described here has been validated (Wang et al., Ann Intern Med 2022; 175:344-351).
2. The right IJV is imaged transversely just above the clavicle of a sitting patient using MINIMAL pressure with the linear probe.
3. Normal (or low) RAP produces a flattened IJV that always contains some blood. The IJV collapses at least subtly soon after the start of each carotid pulsation (systolic collapse) because this is when the atria fill. Inspiration also decreases the size of the IJV.
4. Elevated RAP produces a distended, rounded IJV. A distended IJV has a diameter of at least ¼ the diameter of the IJV during a Valsalva maneuver. The following clip shows a normal IJV followed by a Valsalva maneuver.
5. An exam of a sitting patient less than 6 feet tall that shows a non-distended IJV just above the clavicle concludes: “JVP is not elevated.”
6. Patients taller than 6 feet should be examined halfway reclined so that modest JVP elevation is identified. A non-distended IJV in this position means “JVP is not elevated.”
7. If a patient has a distended IJV above the clavicle, slide the probe cephalad with minimal pressure until the distention disappears. It is good enough to describe such a patient semi-quantitatively as “JVP was elevated to the mid-neck.”
8. When JVP is increased, observe the fluctuations. If the distention increases with inspiration, the patient has a Kussmaul sign, indicating a significantly abnormal right heart, including tamponade. The following clip with Color is from a patient with tamponade. It began with a distended IJV while the patient inhaled, then the IJV deflated when the patient exhaled.
INFERIOR VENA CAVA (IVC)
We assess this vein when fluid tolerance is a clinical question. Remember that identifying fluid responsiveness, as discussed with the dynamic carotid flow time, is usually more valuable than fluid tolerance.
IVC assessment is less helpful in identifying high RAP, including tamponade, although a rounded and enlarged IVC is expected with these conditions. The IVC usually fluctuates in size with RAP, but the absolute IVC lumen diameter is unreliable because of inter-patient variability; normal people can have good-sized IVCs. Of greater value is the variability of the IVC with respiration. Negative intrathoracic pressure from inspiration normally causes a transient decrease in the diameter of the IVC lumen close to the heart if the RA can accept more blood.
First, assess the IVC with a short-axis view 3-4 centimeters caudal of the RA. The phased array probe is probably best, but the curvilinear can be used. Begin with a subcostal4 heart view and center the right atrium. Then, fan down until the probe is vertical and image the short-axis IVC 3-4 cm. below the RA. If the IVC is flattened and collapsing with inspiration, the patient should be fluid-tolerant and unlikely to have elevated RAP. No further measurement is needed.
If the IVC is rounder with equivocal inspiratory collapse, a more precise measurement of the variability might be helpful. The long axis view has traditionally been used because the lumen may be more evident. However, before moving to the long axis, notice whether the IVC moves laterally with respiration in the short axis. Such movement can produce artifacts with the long axis assessment.
A 2020 study of sick adult patients (Caplan et al., Ann. Intensive Care 10, 168) showed that 4 cm caudal to the right atrium was the best location for evaluating respiratory variation. All patients were examined with a phased array probe/heart preset in the semi-recumbent position (30-45 degrees elevation). The study used a GE-developed application (Auto-IVC) to measure the variation; this app is now on Venue. A good long-axis view of the IVC, showing its anterior and posterior walls throughout a respiratory cycle, is needed for the app to function. Poor images will not be accepted, and an unsteady probe or lateral movement of the IVC during the respiratory cycle can produce false positive variability.
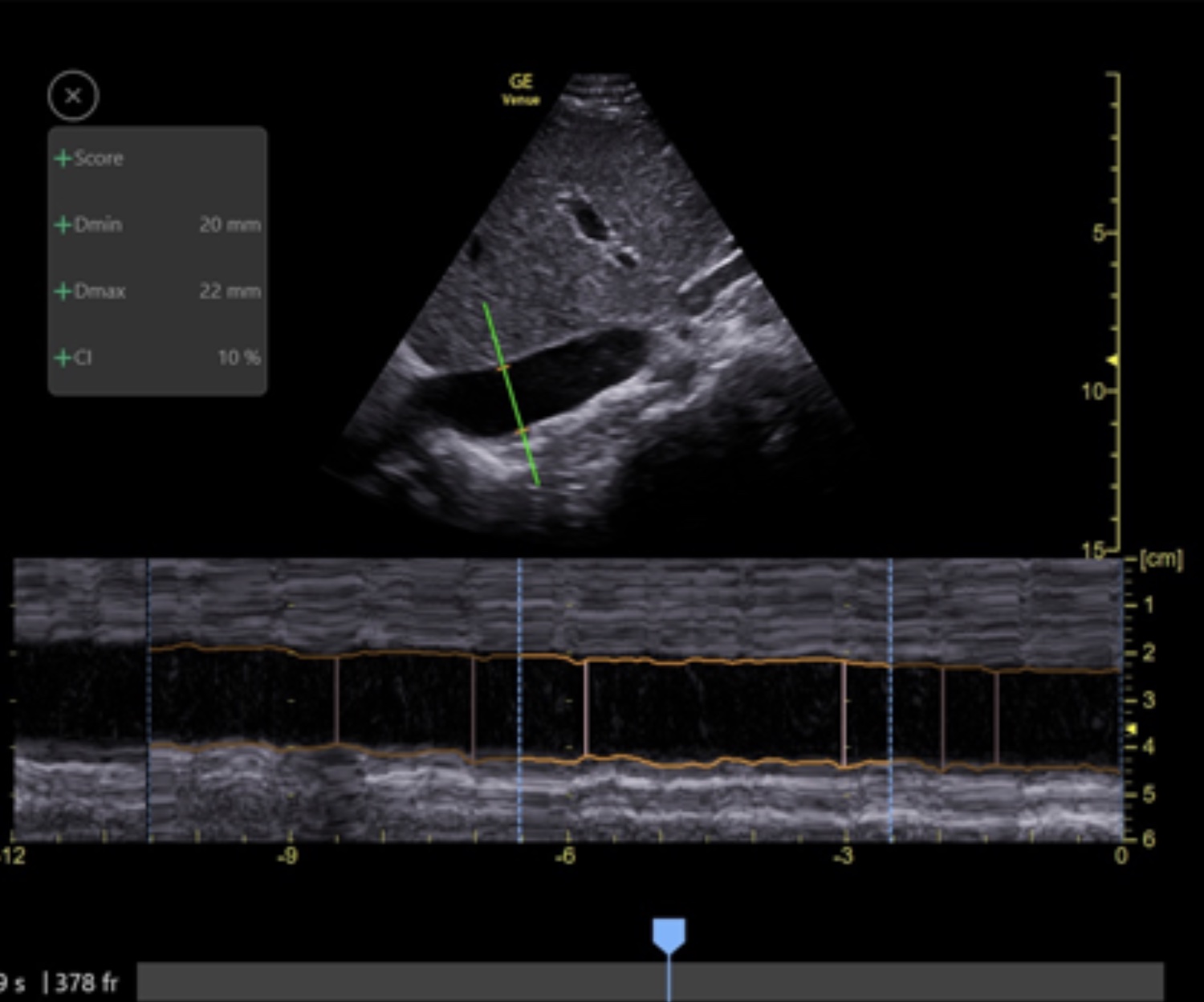
When Auto-IVC is activated, an anatomic M-mode cursor is placed perpendicularly through the IVC, and continuous measurement of the maximal and minimal diameters of the IVC begins throughout 4-second cycles. If necessary, move the cursor to about 4 cm caudal of the RA. GE chose the Collapsibility Index (CI) to express the respiratory variability, and it is calculated as follows:
(1 – Dmin/Dmax) x 100
The following is the output from the Auto-IVC application in a patient with a CI of 10%.
The higher the CI, the more likely a patient is fluid tolerant. In the study, a CI of > 33% in spontaneously breathing patients had a sensitivity of 66% and a specificity of 92% for fluid tolerance. When patients performed a moderate intensity 3-4 second inhalation (not called a sniff), a CI of > 44% had a sensitivity of 93% and a specificity of 98% for fluid tolerance.