Tricuspid Valve
Regurgitation, RV systolic pressure assessment, and the influence on our understanding of central venous pressure.
TRICUSPID REGURGITATION (TR)
TR is the primary concern with the tricuspid valve (TV) because tricuspid stenosis is rare. The TV is more difficult to image than the mitral valve. The PLAXR may see TR well, and although it is not parallel to flow, a rough estimate of the TV gradient can be obtained; it may take a slightly more cephalad apical window to see the TV well in the apical4. The apical3R is excellent for TR because it is parallel to flow but has an anterior/posterior viewing plane through the valve that can be better for many patients.
Trivial TR is common, and functional TR (caused by RA or RV enlargement) is more frequent than primary structural TR. Twenty percent of RV pacemaker leads cause TR, and this can be a nidus for endocarditis. The quantification of TR is similar to that of AR and MR. As with other valve lesions, the patient's preload, afterload, and contractile state will vary the apparent severity of the TR. Chronic, severe TR should have a dilated right atrium and coronary sinus, as well as abnormal IVC and IJV. Eventually, with ≥ moderate TR, the RV will dilate and have decreased function because of the volume overload. TR that is ≥ mild should be followed periodically with IMBUS for progression. Valve centers are becoming more aggressive in correcting TR with new transvenous approaches because mortality increases with the severity
TR Classification |
Mild |
Moderate |
Severe |
Flow convergence |
Minimal to none |
Detectable but small |
Prominent |
Vena contracta cm |
thin |
medium |
wide |
Jet area |
Small, < 20% RA area |
In between |
Large, > 40% RA area |
The following patient had a pacemaker and mild TR, as seen in this PSAX.
Next is the same patient with a view from the apical4 where the TR is more impressive around the pacemaker.
Here is a final view of the TR in the same patient from an apical3R view. Again, the TR nicely courses along the pacemaker lead.
Next is a patient with ≥ moderate TR in the PSAX. There is also some central AR seen.
The following patient had an eccentric TR jet that showed best in the subcostal4. The Color sector box needed to be a little wider to see the proximal part of the TR on the RV side.
The remaining TR examples will be in the apical4. The first is a central TR jet with a definite but small convergence zone. The jet is not large, so this is the beginning of moderate. The right atrium is not enlarged.
The following clip is the B-mode image in an apical4 that should have had less depth, but the view is nevertheless good. The thing to notice is the atrial septal aneurysm bulging into the LA because the RAP was higher than the LAP.
When Color was applied, TR was seen with a large convergence zone, thick vena contracta, and a long, aliased jet moving eccentrically along the inter-atrial septum, pushing the RA into the LA during RV systole.
This penultimate case has a large convergence zone and thick vena contracta with a strongly aliased jet. This would be entering the severe range for TR.
Finally, here is another severe TR with a large convergence zone, thick vena contracta, and a wide jet
TRICUSPID VALVE GRADIENT MEASUREMENT
Severe TR from a structural lesion does not necessarily produce severely increased RV and pulmonary artery pressures. When pulmonary hypertension develops, from whatever cause, the elevated RV pressure begins to push on the tricuspid valve, but the amount of TR may be mild despite high pressures. Nevertheless, the TR jet velocity can be measured and reflects the RV systolic pressure. Measure the jet in multiple views to increase the chance of finding the maximum velocity.
A small TR jet with a uniform blue color usually indicates a low-velocity flow inconsistent with a high gradient between the RV and RA. However, even trace TR jets should be analyzed so that you develop competence in measuring TR gradients.
Position the continuous wave Doppler gate line parallel to the TR jet flow with the area of interest in the vena contracta of the jet. We want the maximum gradient, which should be with inspiration, but use expiration if that is a better view. Here is a good tracing with the peak velocity measured and the gradient calculated. To be picky, the peak was probably over-measured by about 0.3 m/sec because the cursor was placed toward the tip of the “beard” and not at the more defined “chin.”
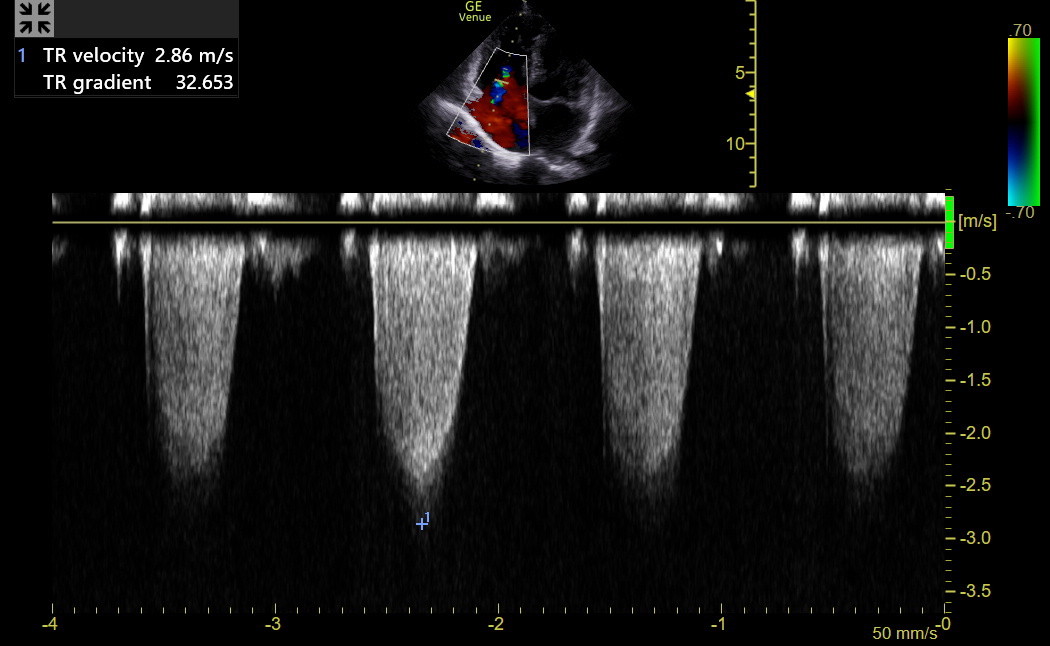
A clear spectrum is necessary for accurate measurement. Freeze and measure the depth of the most prominent negative spectrum. In the above example, the maximum velocity was 2.9 m/sec, with a gradient of 33 mmHg.
Traditionally, estimated right atrial pressure, based on the IVC, was added to the tricuspid gradient to calculate peak RV systolic pressure. However, most experts realize the inaccuracy of this estimate, so the emphasis has now shifted to using the TV gradient alone. The TV gradient has an upper limit of normal of about 21 mmHg and an equivocal range of 22-27. TV gradients greater than 27 mmHg are seriously concerning for pulmonary hypertension (if pulmonic stenosis is excluded).
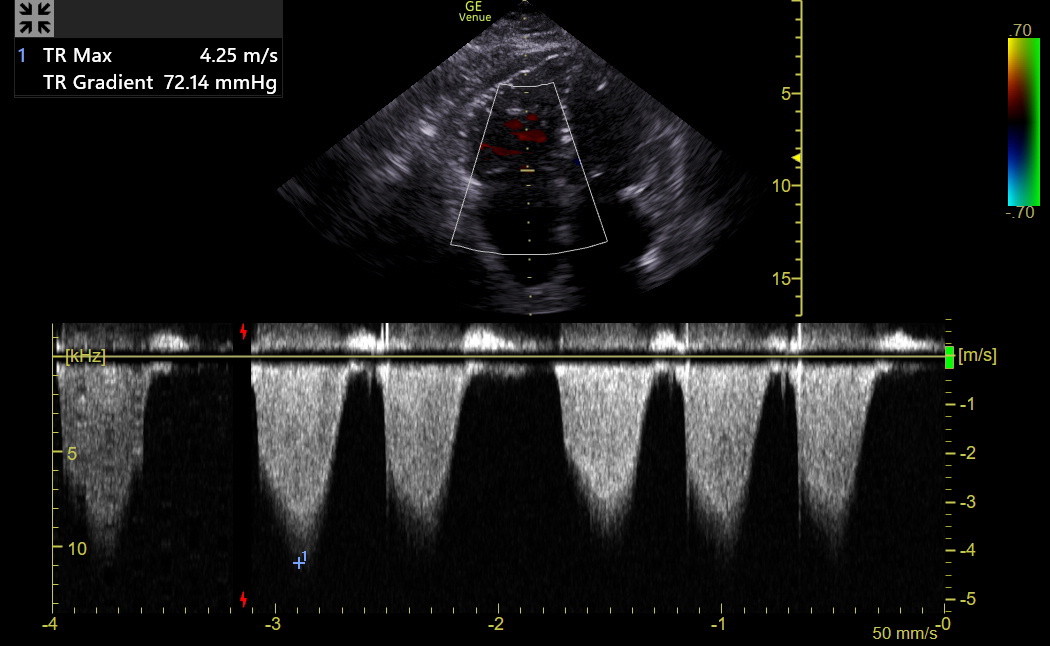
Here is a CW spectrum from another patient whose peak velocity was 4.25 m/sec (a peak gradient of 72 mmHg). This is a substantial elevation in RV systolic pressure.
In the most severe TR, the continuous wave Doppler spectrum may be triangular-shaped and unreliable for gradient measurement because the pressures in the RV and RA begin to equalize. If the TR spectrum is indistinct, it is also dangerous to make the measurement.
Several factors influence the tricuspid gradient, so the most reliable diagnosis of pulmonary hypertension comes from measuring pulmonary vascular resistance during a right heart catheter. We want to identify patients with undiagnosed or newly increased tricuspid gradients who need to move ahead with formal echo and then right heart catheterization. The chapter on Advanced Right Heart Disease explores this in greater detail.